Countries prepared for health emergencies
The COVID-19 pandemic has exposed gaps in the way preparedness for health emergencies is measured and strengthened in countries.
Over the past 2 years, WHO worked with countries and partners to improve how health emergency preparedness is assessed, to strengthen national and community readiness and resilience and to advocate for substantially, sustainably increased financing for public health preparedness.
WHO’s support to countries during the early stages of the pandemic was largely made possible by recent progress in assessing and reporting on national preparedness capacities. In 2020 and 2021, WHO continued to support countries in carrying out preparedness assessments, including through the International Health Regulations (2005) (IHR) States Parties Self-assessment Annual Report. A voluntary Joint External Evaluation was conducted in Ukraine in 2021, bringing the total number conducted since 2016 to 114. Both assessments are key elements of the IHR monitoring and IHR monitoring and evaluation framework framework. WHO facilitated 114 intra-action reviews and five after-action reviews to support countries in evaluating their performance during and after health emergencies and to learn from successes and challenges. Member States led 50 simulation exercises during the biennium. WHO will continue to ensure that the results of all preparedness assessments are regularly validated against the actual outcomes of health emergencies.
In line with recent reviews, recommendations and resolutions, WHO is collaborating with national focal points, experts and key stakeholders to evolve preparedness assessment methods to ensure they are more predictive, dynamic and holistic. This progression includes development of the “dynamic preparedness metric”, incorporation of additional indicators, a strong shift to subnational assessments and pilot-testing and introduction of a new peer-review mechanism, the “universal health and preparedness review”, which aims to increase accountability and transparency among Member States. To support links between stakeholders in health security, health systems strengthening, primary health care and universal health coverage, WHO launched the Health Systems for Health Security Framework and published a position paper on Building health systems’ resilience for universal health coverage and health security during the COVID-19 pandemic and beyond. Use of these resources will further strengthen resilience in countries and enable them to “build back better” from COVID-19.
Countries must improve their preparedness and readiness to face the evolving COVID-19 pandemic and inevitable future health emergencies. WHO worked with Member States to use the outcomes and recommendations of assessments to inform actions and to provide targeted support to strengthen capacities that were shown in responding to COVID- to require improvement. For example, WHO supported countries in enhancing risk communication, strengthening infection prevention and control and improving capability at the human–animal interface. Five OneHealth IHR–Performance of Veterinary Services National IHR–Performance of Veterinary Services National Bridging Workshops Workshops and 14 OneHealth joint risk assessments with both the human and the animal health sectors were carried out in 2020–2021. In line with WHO technical guidance and recommended actions, countries continued to scale up preparedness in specific contexts, such as urban settings, small island developing states, cities and conflict settings, building on the Sendai Framework for Disaster Risk Reduction (in line with Sustainable Development Goal 11). WHO has assisted more than 75 countries in developing national national action plans for health securityaction plans for health security, which will be key to improving core capacities, from clinical management and multisectoral coordination to community resilience and health system strengthening. In 2020–2021, the WHO benchmarks for IHR capacity were updated to reflect the lessons learnt from COVID-19 and to recommend specific activities for capacity-building. WHO tools, such as the Strategic Partnership Portal for health security and resource mapping, support countries, partners and donors in aligning their investments with national action plans for health security, which remain substantially underfunded. WHO is working at all levels to enhance multisectoral coordination for preparedness, including through the Global Strategic Preparedness Network.
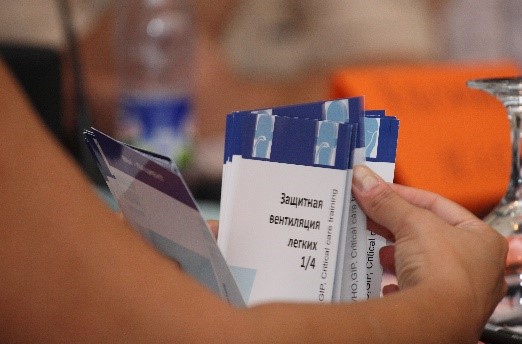
WHO guided and supported countries in improving their dynamic readiness and community resilience for health emergencies. COVID-19 has shown that systems, networks and public health functions must be agile and ready to respond to identified threats. WHO also highlighted gaps in readiness and resilience at community level. With tools, guidance, training, technical support and almost 50 simulation exercises, WHO supported countries in identifying, mapping and mitigating risks and vulnerabilities, including at the human–animal interface, at points of entry, in international travel and transport and at mass gatherings. These activities allowed countries and local communities to anticipate and accelerate critical, tailored activities for operational readiness.
WHO is leading a movement to use a whole-of-society, community-centred, multisectoral approach to health emergency preparedness and readiness. This will require strong systems, governance and financing at national, regional and global levels.
WHO’s response to health emergencies: 2020-2021
WHO'S CONTRIBUTION TOWARDS HEALTH OUTCOMES
WHO's Output Scorecard measures its performance for accountability
The Scorecard below shows the assessment of WHO’s performance in delivering the programme budget outputs agreed with Member States using six different dimensions, i.e., technical support, leadership, global public health goods, value for money, gender, equity, human rights and disability, and achieving results in ways leading to impact. The dimension score (shown as a line) is the aggregate score of the different attributes (shown as sticks). A Scorecard is reported for every output at the global level. In addition, every major office reports its Scorecard for every output.
-
All-hazards emergency preparedness capacities in countries assessed and reported
-
Capacities for emergency preparedness strengthened in all countries
-
Countries operationally ready to assess and manage identified risks and vulnerabilities
SCORING SCALE
View global output leading indicators
Learn more about the Output Scorecard
BUDGET FINANCING AND IMPLEMENTATION
Overview
Within Programme budget 2020-2021, the budget was approved by the World Health Assembly by outcome. Prioritization of work by the countries was also carried out by outcome, as was the development of the bottom-up budget. The result is a strong association between the highest prioritized outcomes and their budget levels – for example the outcomes prioritized as high by country offices were allocated 87% of the budget and 86% of the available funding for country offices.
At the end of the biennium, the overall average financing of the 12 programme budget outcomes was 88% with 3 outcomes funded over 100% and 3 outcomes having less than 75% financing (see Budget section). Disaggregation of financing to the level of outcome and major office shows a number of outcomes with significant underfunding as biennium closed and highlights the chronic lack of sustainable financing to reduce funding gaps. It also underlines the importance of flexible resources, which are key to reduce chronic gaps in certain areas of work. As reiterated within the Sustainable Financing Working group discussions, as long as flexible and thematic funds remain the lesser proportion of resources available, improving allocation of resources can only be successful to a very limited extent.
Additional details for key figures on budget, financing and implementation for the outcome, presented by organizational level (Countries, Regions, Headquarters), contributors, type of expenses and much more can be seen by following the below link.
THE GLOBAL PUBLIC HEALTH GOODS PRODUCED BY WHO
See the list of Global Public Health Goods guiding polices, decisions and operations to drive impact
Select output to view the list