
Ethiopia
Ethiopia, Grade-3 Emergency
- People in need: 28.6 million1
- People targeted: 26.6 million
- People in need of health assistance: 13.1 million
- Requirements (US$): 128 million
Context
The humanitarian situation in Ethiopia remains complex and volatile. The combined effects of the conflict in Tigray, access constraints and the drought affecting the south and southern regions, are hampering the health and well-being of millions of civilians. These factors are also causing internal displacement and enhancing the risk of disease transmission.
Following the signing of the Cessation of Hostilities Agreement (CoA), the humanitarian access situation in Northern Ethiopia is gradually improving. Inland access to Tigray resumed via several corridors and humanitarian flights (both for personnel and supplies) have increased their operations. The improvement of the access situation opens new windows of opportunities to scale up WHO interventions to actively participate in the efforts of reconstruction/rehabilitation of health infrastructure as well as the restoration of lifesaving health services through the prepositioning of medical kits, supplies and commodities.
Acute malnutrition remains a major public health concern. The prolonged drought, especially in the south and southern regions, continues to compromise fragile livelihoods, thereby hampering the existing poor nutritional status. Coupled with food insecurity, disease outbreaks and weakened immunity have increased the risk of morbidity and mortality.
The combined effect of these emergencies is leading to a gradual disruption of the health delivery system. The overstretching of health services in towns and cities hosting internally displaced persons (IDPs) has put the most vulnerable at increased risk of disease and death by common causes of illness. Hard-earned gains in epidemiological surveillance and response, including immunization, might be lost and the risk of outbreaks is high due to overcrowded IDP camps and the disruption of routine immunization. As a result, millions of people have been put at risk of epidemic-prone diseases such as measles, polio, cholera, meningitis, malaria and COVID-19.
Response strategy
To address these emergencies, WHO will collaborate with the Federal Ministry of Health, the Ethiopian Public Health Institute (EPHI), the Regional Health Bureaus (RHBs) and other health partners to expand on current health sector development initiatives and improve response readiness for a further deterioration of the humanitarian situation. At the same time, WHO and its partners will work to increase capacities and incorporate risk management and resilience-building strategies to promote long-lasting solutions to the crisis.
WHO will provide material and operational support to priority health facilities to ensure continuity in the delivery of essential health services, including emergency and trauma services; newborn, maternal and child health services; emergency and essential surgical care; mental health and psychosocial support (MHPSS); reproductive health services and clinical management of survivors of rape and intimate partner violence (CMR/IPV) for survivors of gender-based violence (GBV); the management of severe acute malnutrition (SAM) with medical complications; the detection and management of priority communicable diseases; and the management of chronic diseases.
WHO will support the broader implementation of public health measures to prevent and manage disease outbreaks, with a focus on malaria, cholera, measles, polio, yellow fever, meningitis and COVID-19. To do so, WHO will invest in capacity building of national and local partners, and resume diagnostic testing, vaccination campaigns, mass drug administration and vectors control activities. WHO will also establish and operate dedicated treatment centers and ensure inter-sectoral collaboration with other clusters (especially Water, Sanitation and Hygiene (WASH) and Nutrition) for the physical improvements of shelters, nutrition and WASH. Public health measures for disease control will be integrated within essential health service delivery as well as epidemiological surveillance and early warning mechanisms.
Activities will cover all of Ethiopia, with a particular focus on the conflict-affected regions (Tigray, Afar, Amhara) and those affected by the ongoing drought (with special emphasis on Oromia and Somali regions). Activities will be harmonized with ongoing interventions undertaken by the UN as well as national and local partners and will be aligned with the health cluster’s strategy, as well as with Human Reproduction Programme (HRP)’s country objectives. In this sense, WHO will leverage its role as the health cluster lead to strengthen inter-sectoral coordination and health information systems, with an emphasis on enhancing protection and access to essential health services.
Strategic objectives
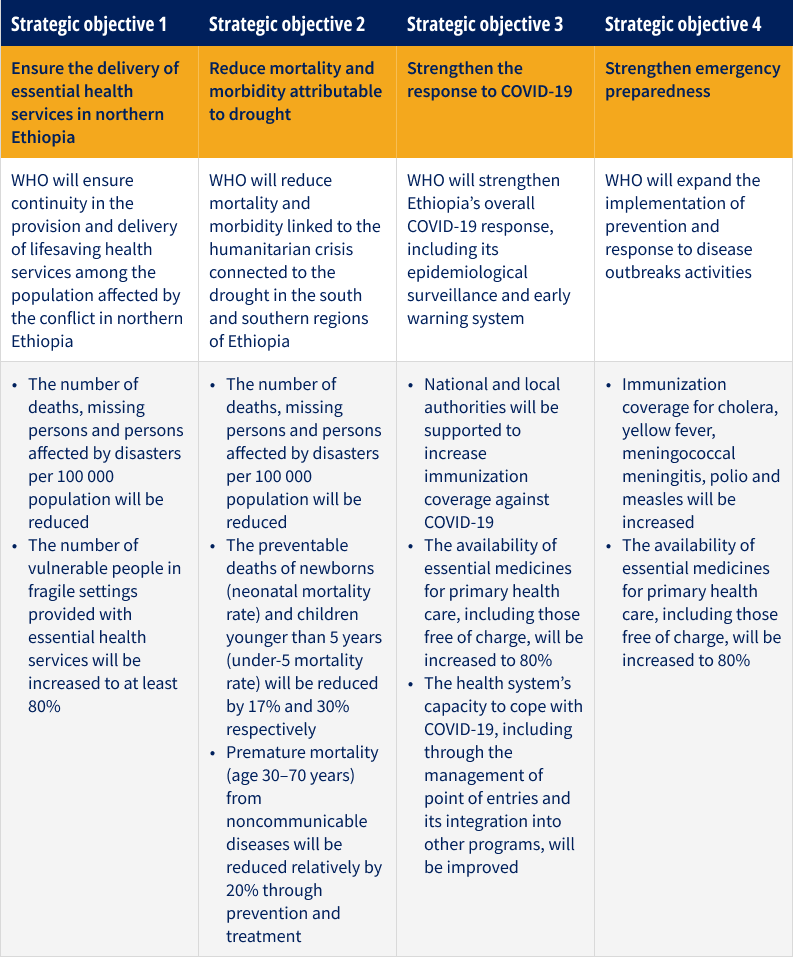
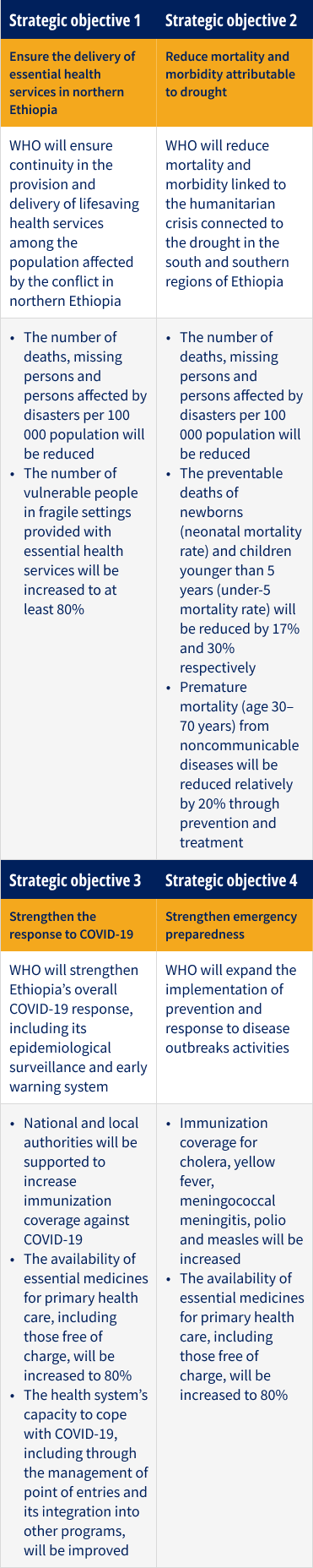
Key activities
- Enhance surveillance capacities to prevent and manage outbreaks
- Provide supplies, drugs and commodities to refill health facilities’ stocks
- Improve the health sector’s capacity gaps by providing training on the Integrated Disease Surveillance and Response (IDSR), the treatment of SAM and MHPSS, the response to GBV and the prevention and response to sexual exploitation, abuse and harassment (PRSEAH)
- Provide support for transition and the integration of COVID-19 response into essential health services and other public health emergency programs
- Support the demand for vaccines thereby strengthening immunization programs and improving vaccination coverage
- Strengthen local partners’ capacities to provide essential health services in the field (e.g. deployment of mobile health nutrition teams (MHNT) and rapid response teams (RRT)
- Lobby with national and local authorities to ensure that hard-to-reach zones are provided with the necessary level of medical stocks and services and
- Leverage WHO’s role as health cluster coordinator to harmonize activities and efforts among health partners
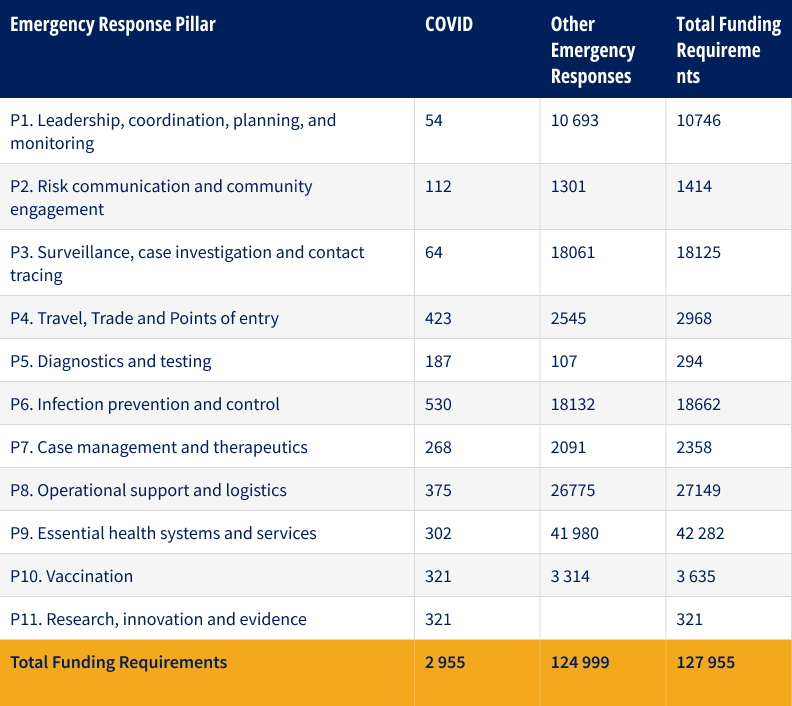
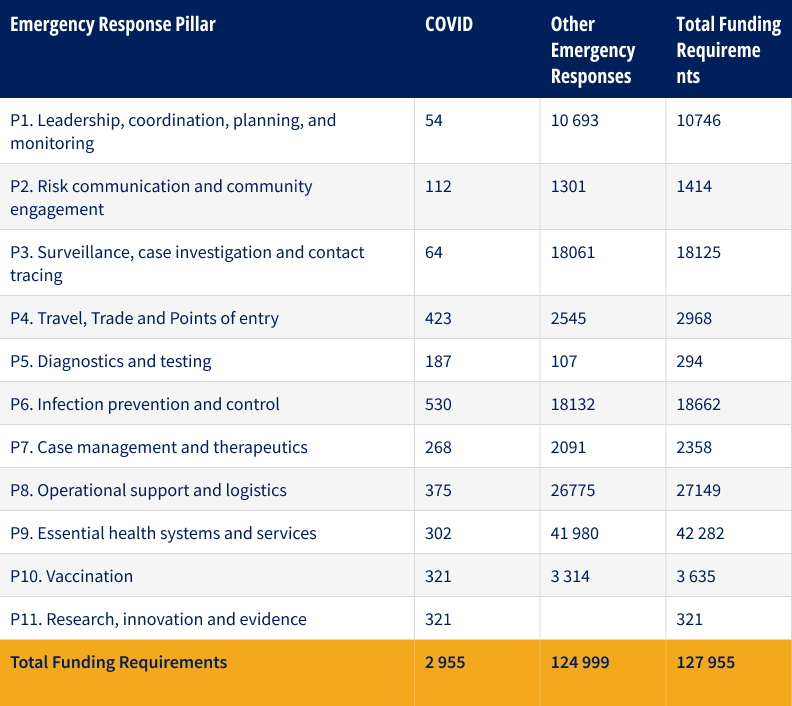
Funding requirements
Overall country funding requirements, including COVID-19, by pillar (US$’000)
Success stories
Voices of the people affected by drought in the Somali Region
In early June 2022, WHO Ethiopia’s Emergency Preparedness and Response team visited the Somali Regional State to provide technical support and oversight of the health response to the severe health consequences of drought and food insecurity in the region. Over 3.5 million people, half of the population in the Somali region, are affected by the drought, whilst malnutrition among children and breastfeeding mothers continues to rise.
The WHO team visited stabilization centers where children with severe acute malnutrition are treated. The team met with several stakeholders caring for children with acute malnutrition, including WHO-trained doctors and nurses at the facilities, caregivers and communities and officials from the Somali Regional Health Bureau.
The mobile health and nutrition team were deployed among the displaced communities to provide health care services within their settlement sites. The communities were made aware of the team’s operating schedule, enabling them to wait under tree sheds to receive health services.
Hope and restoration at Gode Hospital where ailing children receive life-saving treatment
When her 11-month-old son, Abdulnasir, refused to breastfeed or eat his food, Amina knew something was seriously wrong with him. He had had diarrhea, vomiting and fever for more than a week, but it was when he kept crying in pain, stopped feeding altogether and got very weak that she got alarmed and brought him to Gode Hospital in Somali Region. Following a thorough examination upon arrival at the hospital, Amina was informed that her baby was suffering from severe acute malnutrition (SAM) with dehydration due to diarrhea and vomiting and that he would need to be admitted to the SAM Treatment Center at the hospital. Dehydration is one of the common medical complications in children with severe acute malnutrition, contributing to morbidity and death.

Abdulnasir is recovering from acute malnutrition at Gode Hospital SAM treatment center. He is now strong enough to breastfeed and take semi-solid foods. WHO provides medical supplies to the treatment center.
Photo Story: World Health Organization Ethiopia joins Emergency Response to Contain the Cholera Outbreak
World Health Organization (WHO) Ethiopia has joined Ethiopia's health authorities in their emergency response to a cholera outbreak in Harena Buluk and Berbera Woredas in the Oromia region.
On 14th September 2022, the first cases of cholera were reported to the WHO Ethiopia Country Office after four stool samples with culture grown for vibrio cholerae were tested. In response, WHO Ethiopia, Oromia Region Health Bureau (ORHB) and Ethiopian Public Health Institute (EPHI) dispatched a multidisciplinary rapid response team (RRT) to the two Woredas. The team arrived on the scene on 16th September 2022, within 48hrs after it was first reported.

For more information
atrick Abok | WHE Lead | WHO Ethiopia | abokp@who.int
Dr Boureima Sambo | WHO Representative | sambob@who.int

WHO is scaling up its operations in eastern Africa as the region faces acute food insecurity caused by conflict, extreme weather events, rising international food and fuel prices and the impact of the pandemic.

WHO with partners and Somalia’s health ministry, visit around 300 000 households every month in drought-affected districts to identify and treat sick children.

