
Libya
Libya
- People in need: 2.47 million1
- People targeted: 800 000
- People in need of health assistance: 3.8 million
- Requirements (US$): 25.3 million
Context
This past year has continued to challenge Libya’s already fragile and severely damaged health system. Health care continues to be the most significant need for many people, particularly non-Libyan migrants and refugees who lack sustained access to primary and secondary health care. This includes limited access to appropriate health care for chronic and infectious disease, obstetric complications and mental health conditions and disorders.
In addition, the COVID-19 pandemic has exacerbated the system’s fragility, highlighting issues such as poor capacity and uneven distribution of the health workforce; chronic shortages of medicines, equipment and supplies; and the paucity of public health facilities that offer a standard package of essential health care services.
In 2021, reports indicated that up to 90% of primary health care (PHC) centers were closed in some areas. One-third of all health facilities in the south and east of Libya were not functioning and 73% in the south and 47% in the east were functioning only partially, mainly due to shortages of staff and medical supplies. Of the total number of health facilities assessed in 2021, 37% were reported to be either fully or partially damaged. The situation is even more critical in remote and hard-to-reach areas. Over the course of 2022, there have been recurrent surges of COVID-19 cases, and reported shortages of routine vaccines, life-saving medicines and human resources in health facilities across the country.

WHO donates ambulances to the MOH to support emergency referral services.
Emergency response
WHO coordinates the health sector’s humanitarian response and continues to work across the political divide to help Libya rebuild its health system.
Libya remains one of the most vulnerable countries in the region due to the presence of foreign armed groups, trafficking of drugs and migrants, uncontrolled borders and organized crime and corruption. Some areas are still difficult to reach, making it challenging to assess needs or distribute supplies. To address this, WHO relies on its network of locally recruited representatives, including field coordinators, infection prevention and control officers and mobile medical teams. These representatives have access to restricted areas, and can therefore monitor the distribution of supplies, and confirm they are effectively going to the areas of greatest need. This provides clear added value for WHO’s activities, particularly as the country faces a new wave of polarization driven by political leadership.
As a result, WHO’s emergency response operations cover all 22 districts in Libya. WHO provides fully equipped health facilities and deploys emergency medical teams across the country, mainly in areas where there is an acute humanitarian need. WHO’s humanitarian assistance accounts for over one third of all health sector medical procedures and consultations.
Strategic objectives
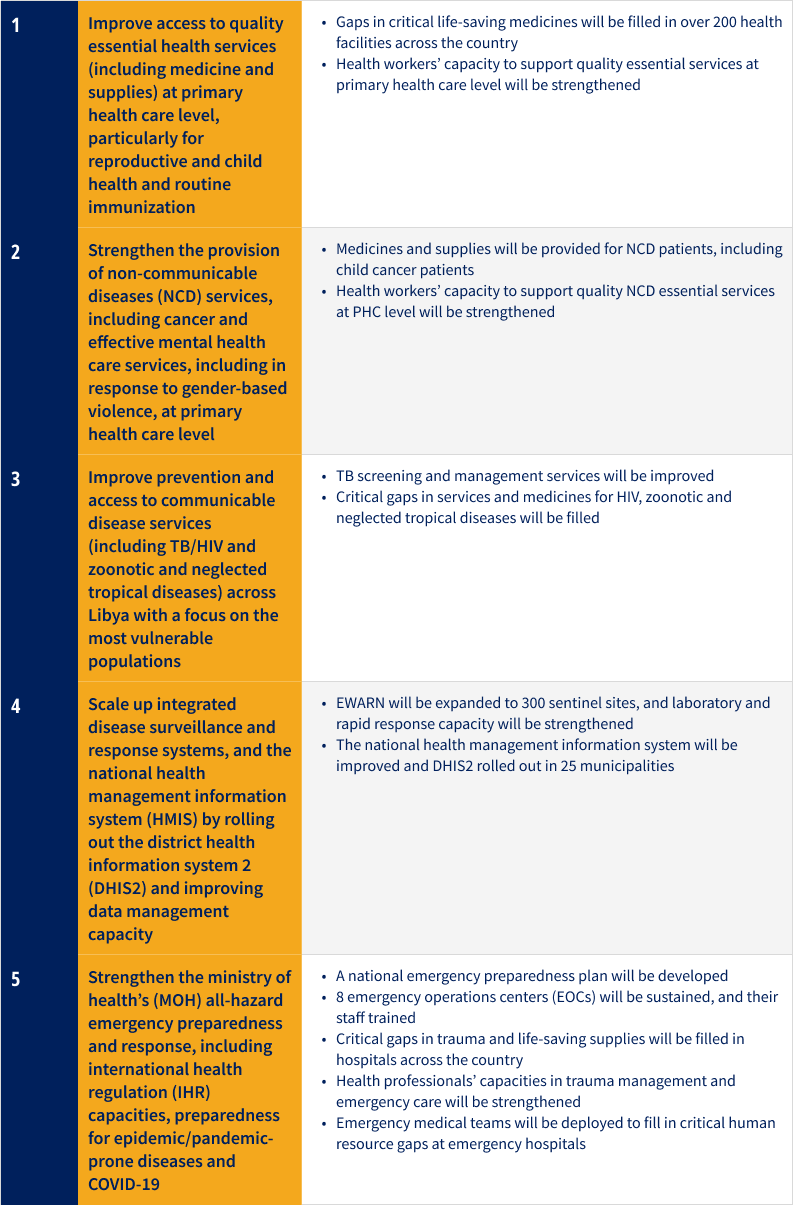
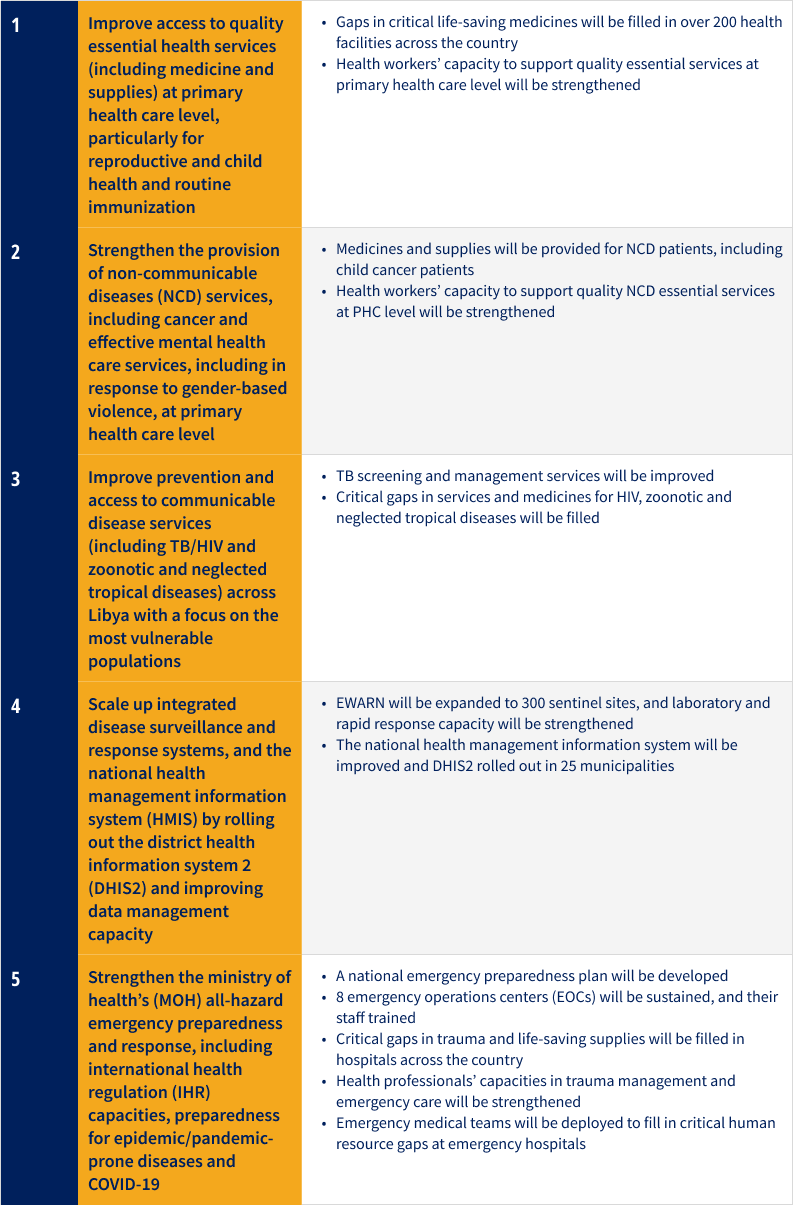
Key activities
- Advocate for and provide health service delivery and technical support, capacity building, training and rehabilitation services; working with health partners; facilitating outreach activities; conducting monitoring and supervision activities and building health information systems.
- Collaborating with national health authorities to support strategic planning, provide technical advice, strengthen disease surveillance, train health care staff, assess health needs and provide medicines, equipment and laboratory supplies to keep essential health care services running.
- Act as the United Nations technical adviser on COVID-19 in Libya, briefing the international diplomatic corps on the status of COVID-19 and immediate needs, obstacles and gaps.
- Collaborate on behalf of Libya with other international mechanisms set up by WHO and partners to tackle the pandemic at the global level.
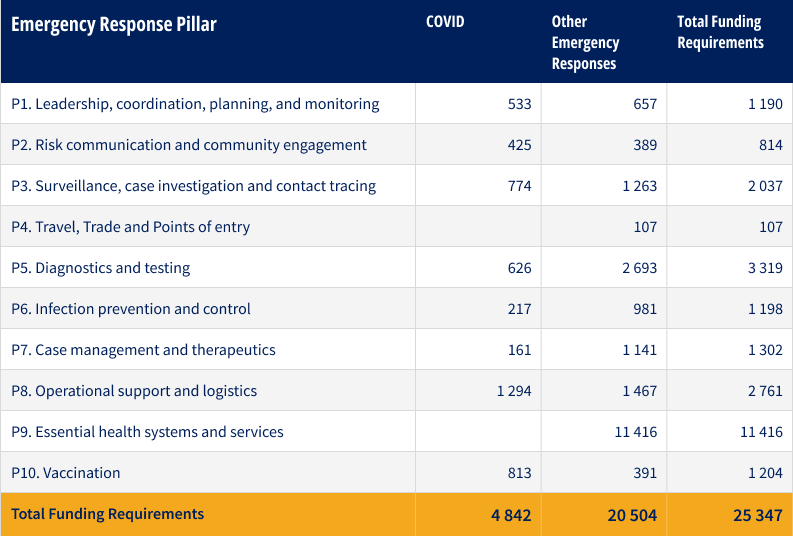
Funding requirements
Overall country funding requirements, including COVID-19, by pillar (US $ million)
Success stories
Mental health and psychosocial support training to help transform mental health services in Libya

WHO-supported mobile medical teams provide essential health services and promote COVID-19 preventive measures.
Armed conflicts cause significant psychological and social suffering to affected populations, with the incidence of mental health conditions more than doubling as a result. The conflict in Libya during the post-revolution period has led to the flow of thousands of cases to the limited number of the existing mental health facilities across the country. Service providers have not been able to cope with the urgent need given the lack of service capacity.2
Beyond this, COVID-19 has led to increased levels of anxiety, vulnerability and psychological stress among all parts of the population. COVID lockdowns and curfews have further exacerbated these challenges given people's reduced access to primary health care (PHC) centers, which are the common entry point for identifying and referring patients who need mental health care. It is currently estimated that approximately one in seven Libyans - nearly one million people - require access to mental health services.3
To help support the strengthening of mental health services in the country, WHO Libya has committed to continue training general practitioners (GPs) on mental health and psychosocial support (MHPSS). Currently, over 150 GPs in 30 PHC centres are offering MHPSS services.
WHO is also working to support improved access to mental health services among young people in school settings. 30 schools in Libya are currently implementing the WHO School Mental Health Package which aims to develop the skills of teachers, social workers and counsellors in recognizing young people’s needs. Approximately 150 staff have been trained so far.
For more information
Ms Elizabeth Hoff | WR WHO | WHO Libya | +41795068721 | hoffe@who.int
Ms Hala Khudari | WHE Team Lead | WHO Libya | khudarih@who.int

