
Uganda
Uganda
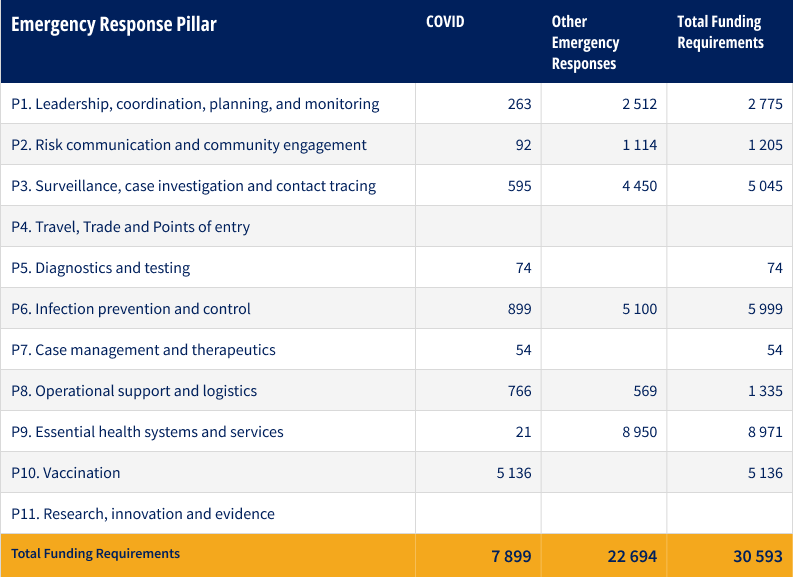
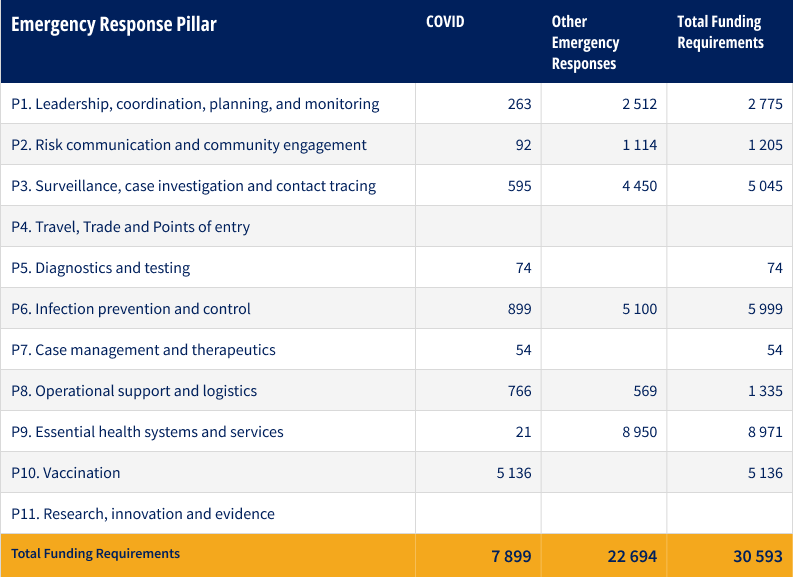
- Requirements (US$): 30.6 million
Uganda is epidemiologically vulnerable to public health emergencies arising from its geographical location in the meningitis and yellow fever belts, the ‘filo virus triangle,’ and proximity to the biodiversity-rich ‘hot spot’ of the Congo basin. It registers the second largest number of public health emergencies in the Africa region annually and is the largest refugee hosting country in Africa, currently hosting over 1.53 million refugees.
Malaria remains Uganda’s leading cause of death, especially in children under five. In 2022, Uganda also saw outbreaks of Rift Valley fever (RVF) and Crimean-Congo hemorrhagic fever (CCHF).
The country is currently responding to two Grade 3 emergencies: the drought in the greater Horn of Africa and COVID-19. The Ministry of Health and its partners are actively implementing public health and social measures against COVID-19, though community adherence has remained low. As of November 2022, 58% of the population was fully vaccinated and 23% partially vaccinated.
On 11 January 2023, the Ministry of Health (MoH) of Uganda declared the end of the Ebola disease outbreak caused by the Sudan ebolavirus that affected nine districts. A total of 164 cases (142 confirmed, 22 probable) with 77 deaths (55 among confirmed cases and 22 among probable cases) were reported during the outbreak.
Although the outbreak has been declared over, health authorities are maintaining surveillance to rapidly identify and respond to any re-emergence. A follow-up programme has been put in place to support survivors. Neighbouring countries remain on alert and are encouraged to continue strengthening their capacities to detect and respond to infectious disease outbreaks.
WHO and partners are continuing to bolster the efforts of the national health authorities to strengthen medical and psychosocial support to Ebola survivors and help them return to a normal life.
Uganda is classified by the International Health Regulations (IHR) as a state infected with circulating vaccine-derived poliovirus type 2 (cVDPV2), with or without evidence of local transmission.
Despite its agricultural potential and significant exports, Uganda’s food insecurity levels remain classified as ‘serious’ by the 2019 Global Hunger Index, and malnutrition is widespread across the country. 1.2 million people in the Karamoja region (Eastern Uganda) are facing severe public health consequences from the deteriorating drought situation and at least 42% (520,000 individuals) are experiencing high levels of food insecurity (IPC Phase 3 or above). Poor rainfalls, below average crop production, recent intensification of cattle rustling associated insecurity and increased national food prices for most of the staple foods associated with the post COVID 19 emergency are also worsening the situation.
Uganda is also prone to disasters caused by natural hazards and epidemic outbreaks. Devastating floods struck the country in 2022, displacing 65,000 people and affecting a total of nearly 300,000.

Members of SUDV contact tracing team preparing to leave for various villages in Mubende district after a briefing at Mubende district headquarters on 30th September 2022.
Response strategy
In line with the National Response Plan for SUDV, WHO aims at stopping virus transmission through scaling up effective, evidence-based outbreak control measures; and preventing its spread to the neighboring at-risk districts through strengthening epidemic preparedness and response measures.
WHO will strengthen traditional coordination mechanisms for epidemic preparedness and response at national and sub-national levels, which provide sustained oversight of public health actions during peace and outbreak response times. WHO will also enhance the functionality of the National Task Forces and District Task Forces and support capacity building for District Rapid Response Teams and national and sub-national teams to effectively manage the surveillance system. To ensure a uniform approach, the Ministry of Health and partners will be supported to roll out the Integrated Disease Surveillance and Response (IDSR) in all districts and cities. WHO will also strengthen the community-based surveillance approaches through Village Health Teams which oversee the implementation of care to patients.
A centralized data and information management system, coordinated by the Ministry of Health, will continue to receive support from WHO. The DHIS 2 platform is a vital aspect of the national surveillance system and WHO will address the unmet need to translate data from the various sources into information products and policy briefs.
WHO will support medical countermeasures (MCMs) stockpiling and capacity strengthening for MCMs management, through making plans and policies available and physically prepositioning and well managing supplies.
Finally, WHO will support progress monitoring in the implementation of International Health Regulations (IHR), including through State Party Annual Rep
Strategic objectives
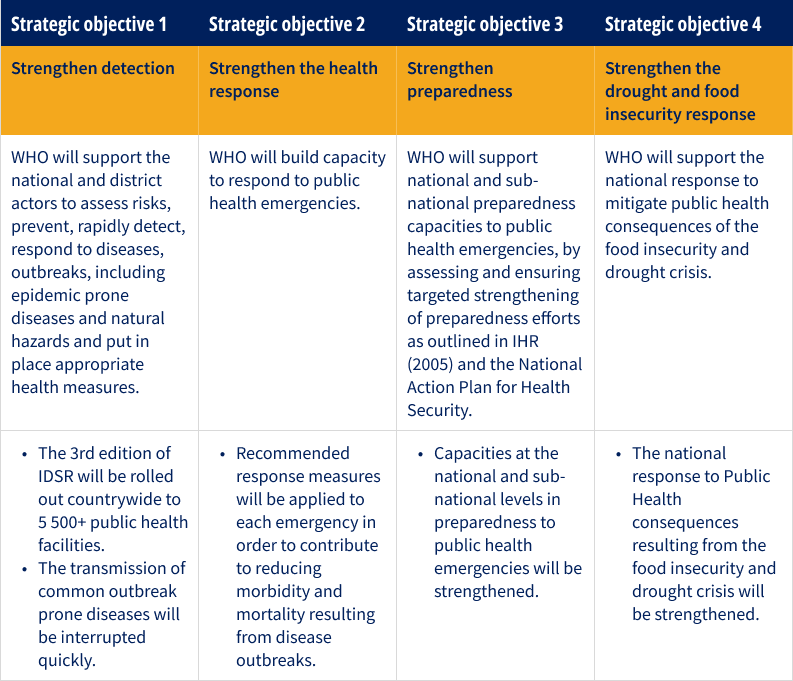
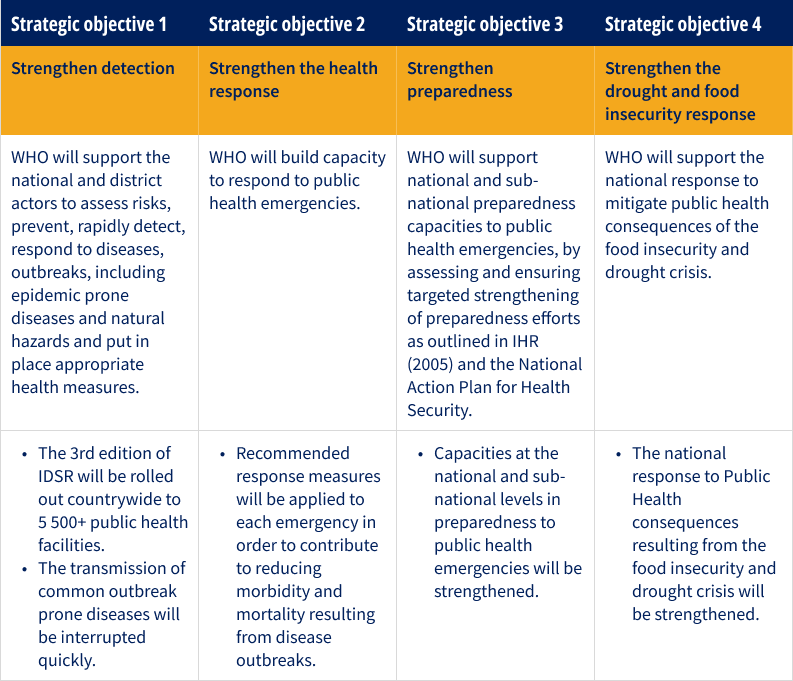
Key activities
- Submit States Party Annual Reporting
- Implement the National Action Plan for health security
- Develop a concept of operations for rapid response teams
- Conduct other IHR monitoring activities
- Conduct simulation exercises and after-action reviews
- Review national risk assessments and develop contingency plans to mitigate outbreaks, including for ongoing Grade 3 responses
- Functionalize the system for rapid risk assessment
- Support capacity development for district and national task forces
- Mobilize and train Rapid Response Teams (RRTs)
- Support regional IDSR focal points operations
- Support the rolling out as well as supervision and monitoring of the IDSR at the district level
- Support epidemiological field investigations and community-based risk assessments
- Develop a food safety surveillance system
- Support sub-national level laboratory capacity, preposition essential diagnostic reagents and transport media for common pathogens, support sample referral, packaging, transportation and testing
- Consolidate and develop a national Infection Prevention and Control program
- Develop contingency plans for chemical emergencies and mass causality management
- Deploy national Emergency Medical Teams and support them through capacity building activities
- Preposition emergency medical countermeasures and mobile isolation facilities
- Complete multi-sectoral response plans and establish effective coordination mechanisms
- Support public health communication during emergencies
- Support response to floods, droughts and mudslides
- Support supply chain management for emergency commodities
- Support the implementation of the refugee response plan, and support the transition from acute emergency to recovery from emergency situations

Members of the Contact Tracing and Risk Communication teams discussing the signs and symptoms of SUDV with the community in Madudu - Mubende District of Uganda.
Funding requirements
Overall country funding requirements, including COVID-19, by pillar (US$’000)
Success stories
Contact Tracers and Village Health Teams Take on SUDV in Uganda
Contact tracers are crucial to ending the spread of SUDV which causes Ebola. Since an outbreak was declared in September 2022 in Uganda, around 300 contract tracers have been deployed to assess if contacts are displaying Ebola disease symptoms. Each tracer works with up to 10 village health workers from the local communities; these are volunteers trained in disease surveillance and recruited to help build trust and overcome fear among communities.
Health assistant Nyangoma Kirrungi is a contact tracer in Madudu sub-county. On average, she follows up on 40 contacts a day. "I work closely with the investigation unit,” she explains. “Once they record a confirmed case of Ebola, my team and I go to the field to follow up with the patient's contacts to ensure that they are symptom-free and then we remain on alert to identify and report symptoms should they develop."
Communities can report suspected cases using two hotlines. Once a case is confirmed, a case investigation team establishes a list of contacts who are then located and screened. Village health teams take over the monitoring of any symptoms for 21 days ‒ the Ebola incubation period – and provide invaluable assistance in raising awareness within their communities. “When the community cooperates in the response and contacts are identified, it becomes easier to contain the disease," says Dr Bernard Logouomo, the Ministry of Health Surveillance Team Lead in Mubende District, another Ebola-hit area.
Since the start of the epidemic, the Ugandan Ministry of Health has trained over 1,200 village health team members with support from WHO. By mid-October, nearly 94% of 552 contacts were seen and monitored daily for 21 days.
Contact tracers and village health teams, however, face numerous daily challenges, including a lack of personal protective equipment, reliable transport and difficulties in monitoring contacts who may not be at home when visited. Contact tracers are also often faced with community members’ fear of being stigmatized or isolated in a health facility, which may put their livelihoods at risk.
With support from the United States Agency for International Development and the Norwegian government, WHO has provided four Ebola kits to Mubende Regional Hospital and redeployed 108 technical staff to assist with case management, risk communication, community engagement and laboratory testing.
For more information
Dr Yonas Tegegn Woldemariam | WHO Representative, WHO Office Uganda | tegegny@who.int

