Mpox Q&A: What you need to know about mpox
3 April 2025 | Questions and answersWithin the last 3 years, WHO has declared 2 global public health emergencies of international concern (PHEICs) for mpox (formerly known as monkeypox). The first PHEIC was declared in July 2022 and lifted in May 2023. With the emergence of a new mpox strain and increased spread in Central and East Africa, a second PHEIC came into effect from August 2024 and is still ongoing. One strain of mpox (clade IIb) continues to circulate in the WHO European Region whereas new strains have been largely limited to imported cases (clade Ia and Ib).
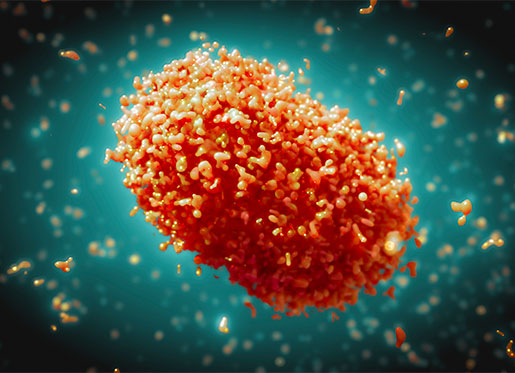
Monkeypox virus (MPXV) has a likely reservoir host in small mammals found in forested areas of Central and West Africa. Since its discovery in 1958, the virus has also been sporadically reported as causing infections in humans through contact with infected animals or from eating infected meat, causing a rash-like illness called mpox disease.
In humans, the most common symptom is an evolving rash on the skin that develops into itchy or painful lesions that can become infected. The rash can affect the palms of hands and the face, mouth, throat, soles of feet, groin, genital areas and anus. This may also be accompanied by fever, muscle aches, chills, exhaustion, headaches, sore throat or swollen, painful lymph nodes (i.e. raised glands, particularly in the groin and potentially in the neck, under the chin and in the armpits). For most people, symptoms will usually resolve on their own after 14–21 days, though some people may require antibiotics and analgesics to treat secondary infections and local pain. In the Region, deaths from mpox are very rare.
Prior to 2022, no known sustained person-to-person transmission of mpox had occurred. However, in May 2022 a large mpox epidemic – not linked to an animal reservoir – emerged in several countries outside of Africa, including in the WHO European Region, with mpox spreading from person to person through skin-to-skin contact, particularly during sex.
In countries affected by the outbreak, most people diagnosed with mpox were men who have sex with men (MSM), especially those with multiple sexual partners.
Transmission may also have occurred, less frequently, through respiratory droplets and contact with contaminated materials.
The virus behind this particular disease outbreak was identified as mpox clade IIb (previously known as West African clade), which usually causes mild disease.
The trend for mpox clade IIb cases in Europe showed a significant rise starting from early May 2022 to a peak in mid-summer (with the PHEIC declared in July 2022), before declining sharply in the autumn. Due to significant progress in controlling the outbreak globally, including in our Region, the PHEIC was lifted in May 2023.
The reasons behind the decline in cases are not fully known, but could include a combination of factors, such as strong intersectoral collaborations, the effective engagement of key affected populations and the community organizations who serve them, public health and vaccination campaigns, as well as behaviour change and the uptake of preventive measures by affected populations.
An upsurge of mpox in the Democratic Republic of the Congo and its spread to neighbouring countries led to the declaration of a second PHEIC on 14 August 2024.
This outbreak was characterized by the emergence of a new virus strain, MPXV clade Ib, spread mainly through sexual activity, but also then within households through non-sexual transmission.
While the 2022–2023 outbreak disproportionately impacted MSM, it is important to stress that mpox can affect anyone who comes into close prolonged contact with an infected person or their infected belongings.
Recent cases of mpox clade I in the Region have originated from people with a travel history to Africa, usually as a result of sexual interaction or other close contact with an infected individual. In a small number of cases, this has then led to transmission to other people in their households, including children.
People at heightened risk of infection include those with multiple sexual partners, including commercial sex workers, as well as health-care workers and close contacts of active cases, such as household members.
Groups at highest risk of severe disease from mpox include pregnant women, young children and people who are immunocompromised, such as people with poorly controlled HIV.
Since 2022 and until the end of March 2025, there have been more than 29 000 cases of mpox in the Region, the vast majority being clade IIb cases. Most of these people recovered from their infection although, sadly, 9 people succumbed to the disease.
During the same period, our Region has seen fewer than 30 cases of mpox clade I, with no deaths attributed to this clade.
A few countries in the Region are still sporadically reporting new mpox clade II cases, predominantly among MSM with multiple partners, however, case numbers remain low.
On 15 August 2024, Sweden became the first country outside the African continent to confirm mpox clade Ib in an individual with a travel history to Central Africa. The confirmation of the case came just one day after WHO’s Director-General declared mpox a PHEIC for the second time.
Since then, there have been occasional imported cases of clade Ib in the Region, in rare situations leading to further household transmission. In February 2025, the first case of clade Ia in the Region was confirmed in Ireland.
Although the numbers affected by clade I in the Region have so far remained low, with most being isolated cases, the fact that the disease caused by this virus strain may be more severe than clade II, or spread more easily from person to person, makes this outbreak concerning.
The recent importations of mpox clade I highlight how this strain could become endemic in the Region if effective measures are not taken to prevent, detect and manage any potential future mpox clusters or outbreaks.
If you are travelling to any of the countries affected by the ongoing mpox outbreaks:
- avoid contact with people who have mpox symptoms
- practice safer sex if you are engaging in sexual activities
- avoid unprotected contact with wild animals (including their meat and blood)
- cook thoroughly any food containing animal parts or meat before eating
- clean your hands frequently with soap and water or an alcohol-based hand rub.
Someone who has contracted mpox usually only starts to show symptoms 6–13 days after their infection, but in some cases, it can take up to 21 days.
If you think you might have mpox or have been in contact with someone who has mpox:
- consult your doctor or health-care provider straight away
- isolate from others until you have been evaluated and tested by health professionals.
If you have symptoms of mpox:
- your contacts and isolate yourself from others until all your lesions have crusted over, the scabs have fallen off and a new layer of skin has formed underneath.
If you are advised to isolate at home, protect those you live with, as much as possible, by:
- asking friends and family to help you by delivering things you need;
- isolating in a separate room;
- using a separate bathroom, or cleaning any surfaces you touched after each use;
- cleaning and disinfecting frequently touched surfaces with soap and water and a household disinfectant;
- avoiding sweeping/vacuuming (this might disturb virus particles and cause others to become infected);
- using separate utensils, objects and electronics, or clean well with soap and water/disinfectant before sharing;
- not sharing towels, bedding or clothes;
- doing your own laundry (lift bedding, clothes and towels carefully without shaking them, put materials in a plastic bag before carrying it to the washing machine and wash them with hot water over 60 °C);
- opening windows for good ventilation; and
- encouraging everyone in the house to clean their hands regularly with soap and water or an alcohol-based hand sanitizer.
The disease is usually self-limiting, which means that symptoms usually go away without the need for treatment within 14–21 days. Some people may require antibiotics and analgesics to treat secondary infections and local pain.
WHO recommends that people at high risk of becoming infected with mpox get vaccinated and complete the vaccination series (i.e. receive all recommended doses). This includes MSM and trans people with multiple male partners, as well as all other people with multiple sexual partners, such as sex workers. Health workers at risk of repeated exposure, laboratory personnel working with orthopoxviruses, clinical laboratory and health-care personnel performing diagnostic testing for mpox and outbreak response team members should also be protected through vaccination.
WHO/Europe encourages countries offering vaccination to ensure equitable and effective access to vaccines for these groups, including by rolling out vaccination programmes in settings, such as sexual health clinics, HIV centres, pharmacies, community-based organizations, sex-on-premises venues and large gathering events, as an effective way to reach many of the highest-risk groups.
Although vaccination is not a silver bullet, it offers an extra level of protection – together with other preventive measures – and reduces the risk of severe disease if infection does occur.
Vaccination is not recommended based on a higher risk of severe disease alone (such as with children, pregnant women and people who are immunosuppressed) unless the group is also at high risk of being exposed to mpox. However, people living with HIV should be considered high priority among these groups.
Vaccines reduce the risks of getting infected. One can become infected or reinfected with mpox after being vaccinated, but vaccines reduce the risk of this happening and reduce the risk of severe disease if infection does occur.
Vaccination can also be offered to prevent infection after high-risk exposure to the virus if given within 4 days of first exposure (and up to 14 days in the absence of symptoms). In case of limited vaccine supply, people at risk of developing more severe disease, if exposed, should be given priority in vaccination.
Eradication means that transmission of a disease has been stopped entirely across the world and there are no longer any cases of the disease anywhere (smallpox is the only disease affecting humans that has been eradicated to date). This is unlikely for mpox because it is a zoonotic disease, meaning it has large animal reservoirs and can spread between animals and people.
In the Region, we are working to eliminate mpox, meaning we want to interrupt sustained local spread, whether it be as a result of sexual or non-sexual transmission.
WHO/Europe’s regional 2023–2027 mpox policy brief – “Considerations for the control and elimination of mpox in the WHO European Region update 25 April 2023: the need for integrated national operational plans” – provides guidance to health authorities and a range of other stakeholders on what actions are needed to control and eventually eliminate mpox in the Region.
This includes:
- integrating the mpox response into national sexual health programmes;
- promoting and bringing testing closer to key affected communities – for example, by offering easy access to diagnostic tests;
- reaching underserved groups – for example, trans people, sex workers, MSM who are also migrants or refugees, as well among younger people, people who are homeless and people in rural areas – with health advice, testing and vaccines;
- declaring mpox a nationally notifiable disease, which will help for early mpox detection, response to outbreaks in a more streamlined way, and an allocation of resources where they are most needed; and
- developing national vaccination plans.
In parallel, it is important for affected populations to continue to stay vigilant – keep up with preventive measures, act quickly if they have or suspect they might have mpox and get vaccines when they are available.
In addition, WHO is working with concerned countries, facilitating information sharing and supporting surveillance, testing, infection prevention, clinical management, risk communication and community engagement.
WHO is also working with vaccine manufacturers to assess the potential for scaling up mpox vaccines and analysing data to see what further measures and strategies should be prioritized to eliminate all mpox local transmission.