The release of a new UN report, Levels and Trends in Child Mortality 2017, has highlighted that every day in 2016, 15,000 children died before their fifth birthday, 46 per cent of them – or 7,000 babies – died in the first 28 days of life.
Levels and Trends in Child Mortality 2017, reveals that although the number of children dying before the age of five is at a new low– 5.6 million in 2016, compared with nearly 9.9 million in 2000 – the proportion of under-five deaths in the newborn period has increased from 41 per cent to 46 per cent during the same period.
Large disparities exist in the survival chances of children aged 5–14 across regions and countries. In particular, the Pacific, excluding Australia and New Zealand, has the second highest probability of children aged 5-14 dying, with 8 deaths per 1,000 children aged 5.
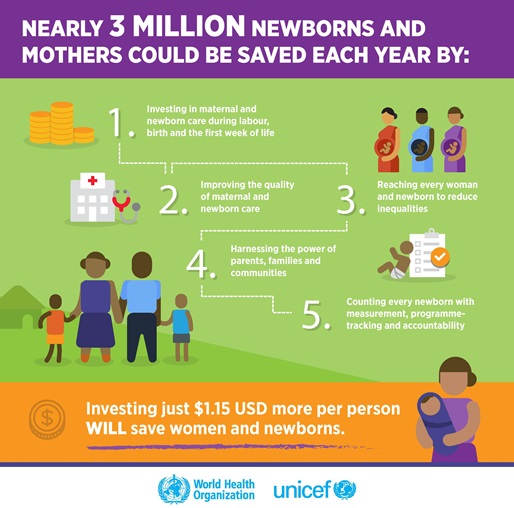
In response to these figures, the report notes that many of these deaths could have been prevented if global inequalities were reduced. If all countries achieved the average mortality of high-income countries, 87 per cent of under-five deaths could have been averted and almost 5 million lives could have been saved in 2016.
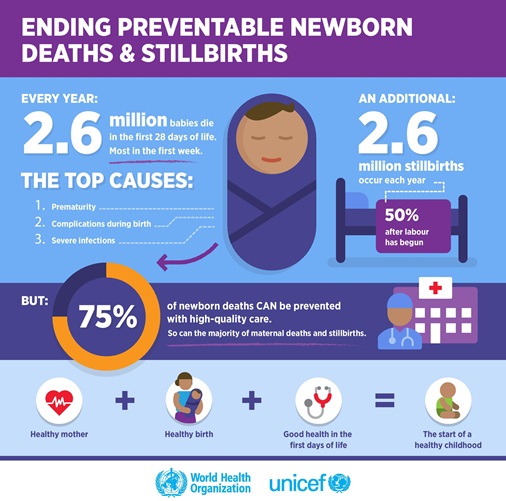
Pneumonia and diarrhoea top the list of infectious diseases which claim the lives of millions of children under-five globally, accounting for 16 per cent and 8 per cent of deaths, respectively. Preterm birth complications and complications during labour or child birth were the causes of 30 per cent of newborn deaths in 2016. In addition to the 5.6 million under-5 deaths, 2.6 million babies are stillborn each year, the majority of which could be prevented.
Ending preventable child deaths can be achieved by improving access to skilled health-professionals during pregnancy and at the time of birth; lifesaving interventions, such as immunization, breastfeeding and inexpensive medicines; and increasing access to water and sanitation, that are currently beyond the reach of the world’s poorest communities.
The WHO works closely alongside Pacific ministries of health and key partners to strengthen Pacific health systems and implement evidence-based policies and strategies for the reduction of maternal and newborn mortality and promotion of adolescent health, including through the implementation of the Baby-Friendly Hospital Initiative (BFHI) in the Pacific.
The BFHI initiative, launched by WHO and UNICEF, is a global effort to implement practices that protect, promote and support breastfeeding. To date the WHO and UNICEF have provided support and encouragement to Pacific ministries of health to establish policies and practices which encourage positive maternal and child health. This includes the promotion of breastfeeding as the only source of food and fluid for a baby within its first six months of life.
At the highest level of accreditation, maternal facilities and hospitals are declared 'Mother and Baby-friendly' when they refuse to accept free or low-cost breast milk substitutes, feeding bottles or teats, and implement 10 specific steps to support successful breastfeeding and safe birthing practices. In 2012 the Solomon Islands’ National Referral Hospital was declared the first hospital in the Pacific to meet expanded standards for both mother and baby friendliness.