In the increasingly interconnected world public health threats have become one of the major global issues. The recent Ebola outbreak has taken more than 11 thousand human lives leaving behind weakened health systems incapable of delivering basic health services without external support1,2. The 2009 H1N1 influenza pandemic killed 284,000 people in its first year alone and the anthrax attacks of 2001 in the USA infected 22 people, killed 5, and cost more than USD 1 billion to clean up. About a decade ago efforts to contain SARS outbreak cost the world $30 billion in only 4 months. Dangers caused by infectious diseases, chemicals, and radiation do not have boundaries and countries must join efforts and work in tandem to ensure health security and safer environment for inhabitants of Mother Earth. Response efforts must be a collective endeavour.
In order to facilitate integrated and collective actions, the International Health Regulations, or IHR (2005), were initiated by WHO. IHR is an agreement made between 196 countries including all WHO Member States to build their capacities to detect, assess, report and respond to public health events. WHO plays the coordinating role in IHR and, together with its partners, helps countries to achieve the commitments made under IHR. IHR coordination is one of the 6 leadership priorities of the WHO programme of work for the next 6 years.
In line with global efforts, regions developed their own collaborative strategies reflecting on specific needs of respective regions. Asia Pacific Strategy for Emerging Diseases (APSED) serves as a common strategic framework for countries and areas of the region to strengthen their capacity to manage and respond to emerging disease threats3.
WHO-coordinated global actions are not limited to technical support only. There are initiatives to mobilize resources to deal with region-specific yet global health security issues. One example of such initiatives is the Pandemic Influenza Preparedness Framework (PIP) approved in 2011 with an objective of improving pandemic influenza preparedness and response, and strengthening countries’ resilience against pandemic influenza by improving and strengthening the WHO global influenza surveillance and response system4.
Mongolia was selected one of the PIP project countries and received funding in 2014, 2015 and 2016. In the country the PIP project was received with appreciation as an opportunity to improve the country’s generic capacity while focusing on influenza.
WHO work on health security in Mongolia
Securing health of the Mongolian population by strengthening the country’s generic capacity to prevent, mitigate and manage public health emergencies caused by any type of hazard (multi-hazard approach) is one of the priority areas of WHO work in Mongolia. WHO support in Mongolia covers all components of emergency management partnering with various agencies. Our partnership goes beyond health sector including animal health sector institutions, state professional inspection agency, emergency management agency, academic, civil society and media organizations. Annual review meetings have become a routine mechanism where all the stakeholders engage in productive dialogue and consultation to reflect on the achievements, identify gaps and determine next steps.

Group discussion during 2016 Annual Planning and Review Meeting. The group members represented the National Emergency Management Agency, National Centre for Communicable Diseases and National Centre for Zoonotic Diseases, Institute of Veterinary Medicine, General Authority for State Inspection, and WHO. January 26, 2016
Predicting potential risks: Epidemiological Intelligence
Being able to “predict or detect” certain risks requires a functioning system able to collect, analyse and distribute related data systematically to inform timely decision-making at an earliest stage of an emergency. Over the past years WHO has continued providing technical and financial assistance to the country in building its surveillance capacity.
Early Warning, Alert and Response (EWAR) system in Mongolia was established in 2009 with WHO support. Data on priority infectious diseases grouped according to set of symptoms are collected every day from each and every primary health care facility and reported to the National Centre for Communicable Diseases weekly. Functionality of EWAR was assessed twice since it started operating. EWAR was later expanded to include event-based surveillance (EBS). Scope of EBS is much broader as it covers not only occurrences of diseases in humans, but also events related to potential exposure for humans, such as deaths in animals, contamination of food products or water, and environmental hazards including chemical and radio-nuclear events. EBS is now an integral part of daily intelligence: on average 300 events are reported per year from various sources including Facebook, social media websites, phone-calls, official sources in other sectors such as animal health, emergency management and inspection. In contrary, syndromic surveillance relies on health facilities only as it is based on clinical manifestations. These two complement each other.
Significant proportion of PIP funds were invested in establishing Emergency Operations Centre (EOC) at the Ministry of Health and Sports of Mongolia and Emergency Operations Points (EOPs) at the NCCD and the National Centre for Zoonotic Diseases (NCZD) through donating equipment, developing standard procedures and training staff.

Dr Soe Nyunt U, WHO Representative in Mongolia; Mr Bat-Erdene, Acting State Secretary; MOHS and Dr. Buyanjargal, Acting Director General Of the NCCD at launching ceremony of EOP at NCCD. December 11, 2015

EOP, NCCD. Meeting with Dr Babatunde Olowokure, Coordinator of ESR/WPR, Mr. Graham Rady, Monitoring and Evaluation Consultant. January 25, 2016
Information collected through the surveillance systems are screened, filtered, presented and discussed during regular joint morning meetings at the EOC and EOPs. Currently EOC/EOPs operate as main resource center where day-to-day preparedness activities such as data collection, analysis, routine risk assessments, communications and information sharing take place.
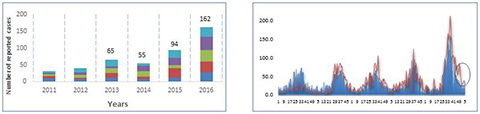
Example of data analysis and discussion during an EOC/EOP morning meeting: Sudden increase of haemorrhagic diarrhoea syndrome reported by weekly EWAR in the first 5 weeks of 2016 compared to the same period the preceding 5 years. Assessing the risk for informed actions
When a surveillance system detects an unusual pattern (for instance: sudden increase beyond threshold or report of an unfamiliar/new disease) its potential risks should be properly assessed to identify if a new situation likely to present serious public health threats of national or international concern. WHO recommends countries to have capacity to conduct such risk assessments on routine basis5. With support from PIP project the MOHS developed and approved the Risk Assessment Guideline adopting WHO recommended procedures.
The MOHS has placed particular emphasis on daily functionality of the Emergency Operations Centre (EOC) as a place for daily risk assessments to inform response actions and risk communication strategies. A more formal process for risk assessments has improved joint risk assessments at the national and sub-national levels and among other relevant sectors and WHO.
 A Risk Assessment Exercise for reported cluster cases of insect bites with 1 death case in Sukhbaatar aimag. EOC peace-time team members, officials from the National Centre for Communicable Diseases and the National Centre for Zoonotic Diseases joined
the session at the EOC, MOHS. August, 2015
A Risk Assessment Exercise for reported cluster cases of insect bites with 1 death case in Sukhbaatar aimag. EOC peace-time team members, officials from the National Centre for Communicable Diseases and the National Centre for Zoonotic Diseases joined
the session at the EOC, MOHS. August, 2015
When the vaccine derived polio (VDP) outbreak emerged in Lao PDR in 2016, the Mongolian MOHS assessed the level of risk of importation and spread in the country. The MOHS led a risk assessment exercise defining a list of risk questions, analyzing baseline data on vaccination coverage, supplementary immunization activity, acute flaccid paralysis surveillance and laboratory-based surveillance. The team involved both technical and managerial experts from various sectors. The risk assessment, as part of emergency preparedness planning, considered the worst case scenario of a polio outbreak and determined the priority of interventions. Although the level of risk was determined to be low, follow up actions and technical recommendations were developed for health facilities at all levels and points of entry. Communication and vaccination strategies were developed in line with IHR Committee temporary recommendations. If a polio case is ever detected in Mongolia, the country will be able to rapidly respond due to the MOHS's proactive preparedness procedures set in place.
The risk assessment procedures have been applied to assess potential risk of events reported since September 2015: 2 plague outbreaks, food poisoning events, potential risk of MERS and Zika, and probable meningitis outbreak. An exercise to pilot use of the same methodology to disaster situation was also organized in February 2016 for assessing likelihood of having health emergencies during 2015/2016 winter-spring period.
Building Response Capacity: introduction of Incidence Management System
If results of a risk assessment indicate level of risk and health consequence to be high a system should quickly respond mobilizing adequate resources to contain a hazard at a minimum cost and minimize its impact. Proper chain of command and control, disciplined and trained staff, adequate coordination mechanism and clear standard of procedures are crucial during an emergency response. Incidence management system (IMS), originated in military, provides framework for standardized organizational structures, functions, and processes for emergency response. After series of training, consultation activities and number of exercises National IMS (NIMS) was introduced in September 2015. The procedure was approved by the Ministerial Order 355.
Since its launch NIMS has been tested during Crystal Exercise for IHR focal points organized by WPRO in December 2015.
 Crystal Exercise -2015. Points of Entries and animal health sector participated in the exercise along with IHR NFP key staff. December 3, 2015
Crystal Exercise -2015. Points of Entries and animal health sector participated in the exercise along with IHR NFP key staff. December 3, 2015
Rapid response teams specific to certain emergencies have been pre-appointed, trained and provided with ‘grab-bags’ where the essentials are packed including smart phones, computers, GPSs, first-aid kits and other survival utensils.
Preparedness at the Points of Entries (PoE) is an important part of emergency preparedness as chances are greater for having imported cases than dealing with cases originated within the country. Cross-border simulation exercises on mutually agreed topics jointly organized with Russia and China’s border quarantine authorities have become annual activities.


Simulation exercise at Zamyn-Uud PoE on scenario of imported H7N7 case followed by visit to China Quarantine Control Department and Isolation Room at Erlian PoE. December, 2014
Competent staff is the most important gear to make the system move forward efficiently. Hence the country program supported establishing Mongolian Field Epidemiologists Training Programme (MFETP), a 1-year programme to train epidemiologists in principles of outbreak investigation, data analysis methods and public health surveillance. So far the Mongolian Field Epidemiologists Training Programme produced over 40 field epidemiologists who upon graduation were appointed as an EOC coordinator, EOP officers and surveillance officers that play key role in public health emergency preparedness.
Ministry of Health and Sports of Mongolia is giving high priority to preparedness by facilitating a successful shift from a reactive response-driven approach to a proactive preparedness. Establishment of network of EOC/EOPs is valued as a key factor that brought preparedness to next level. Hence, the network is planned to be expanded to other sectors namely animal health and inspection.
 Proposed EOC/EOP network, from presentation made by Dr Narangerel, Senior OIC, MOHS during the annual Planning and Review Meeting, 26 January 2016.
Proposed EOC/EOP network, from presentation made by Dr Narangerel, Senior OIC, MOHS during the annual Planning and Review Meeting, 26 January 2016.
_______________________________________
1 http://www.who.int/csr/disease/ebola/en/
2 http://www.globalhealth.gov/global-health-topics/global-health-security/ghsmatters.html
3 http://www.wpro.who.int/emerging_diseases/APSED2010/en/
4 https://www.who.int/initiatives/pandemic-influenza-preparedness-framework
5 https://www.who.int/emergencies/risk-assessments
