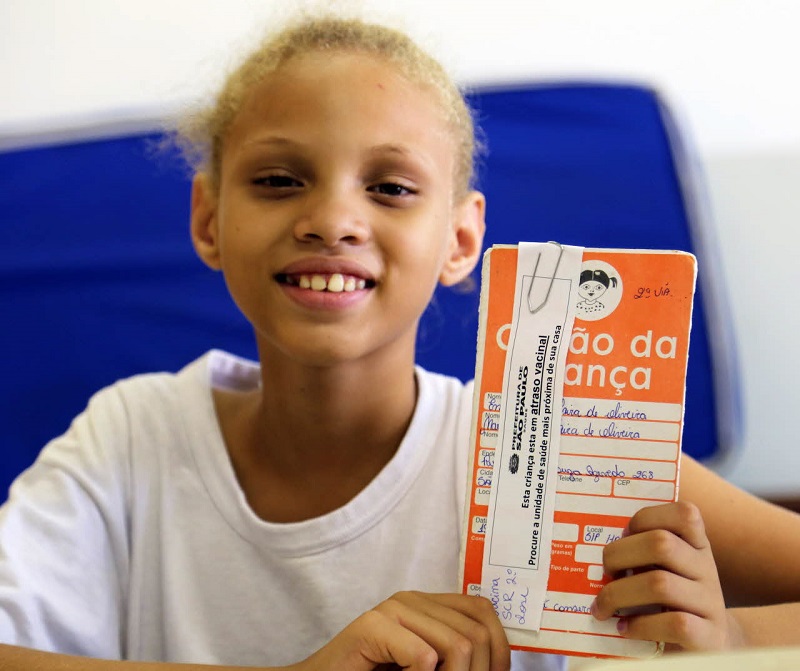
Across more than 80 countries, millions of girls are now able to get vaccinated against human papillomavirus (HPV), substantively reducing their risks of developing cervical cancer later in life.
Modesta is among the many 14-year-olds who have been vaccinated in Tanzania since a national roll-out began in April this year. Together with her best friends, she is now waiting to receive her second dose at a busy clinic in the nation’s bustling city of Dar es Salaam. She explains that she and her parents were happy for her to get the vaccine.
“I’m hoping to become a Health Minister one day”, she says smiling. “And when I do I will make sure that girls of my age get vaccinated against HPV. We are the young and future generation, and HPV vaccine can help us avoid getting sick.”
Spread primarily through sexual transmission, the human papillomavirus causes almost all cervical cancer cases - a disease that too often, affects relatively young women in the height of their productive years. It causes more years of life lost than any other form of cancer, with immeasurable human costs. Every two minutes, somewhere in the world, one woman will lose her life to the disease.
WHO recommends HPV vaccination for girls alongside screening and treatment for older women to reduce their cancer risks. The vaccine is most effective when given early in adolescence between the age of 9 and 14 years – before girls are exposed to the virus.
Vaccination against HPV provides safe effective protection against cervical cancer
Building confidence in the HPV vaccine
Building public trust is a crucial objective of immunization programmes around the world, and this is particularly true when a new vaccine is introduced.
While many countries have achieved high coverage for HPV vaccination, in others, rumours about side effects have eroded uptake. This is despite the fact that such fears have been continuously debunked by scientific evidence. A large body of independent research has shown the vaccine to be extremely safe and highly effective in protecting girls against the most dangerous strains of the virus.
To help combat the spread of such misinformation, WHO has helped countries develop robust public awareness activities, which aim to provide parents, young people, schools and health workers with fact-based information on HPV and cervical cancer. Several European nations including Austria, Denmark and the Republic of Ireland have also formed a peer group to share experiences on effective communications around the lifesaving vaccine.
Such efforts can turn around declines in coverage. In Denmark following a comprehensive national campaign, uptake in the number of girls getting vaccinated is quickly increasing. During the past year, twice as many girls had started their HPV vaccination there compared to 2016.
Reaching the most at-risk countries with HPV prevention
While many wealthier countries now have well-established HPV vaccination programmes in place, a growing number of lower-income nations are preparing to roll it out nationwide. This will be critical for progress, since almost 9 in 10 cervical cancer deaths occur in developing nations.
Negotiated through Gavi, the Vaccine Alliance as well as the Pan American Health Organization’s Revolving Fund, pricing reductions have played a very significant role in expanding access in eligible countries. Including most recently, Tanzania and Zimbabwe, 10 lower-income countries will have introduced the vaccine with Gavi support by the end of 2018, while 10 more hope to follow suit next year.
In each, WHO and other partners are supporting health ministries to identify strategies that will help deliver the greatest possible access and uptake when it is introduced – whether it is made available in schools, clinics or through direct outreach to communities.
Pricing reductions through the PAHO revolving fund enabled rapid access to the lifesaving HPV vaccine in South American countries
“Cervical cancer is one of the greatest killers of women in the world’s poorest countries - yet effective tools exist to beat the disease,” says WHO’s Assistant Director-General for Family, Women, Children and Adolescents, Dr Princess Nothemba Simelela. “We must work together to reach women and girls – wherever they live in the world - with effective, high quality prevention including vaccination, screenings and treatment. No woman should die from a preventable disease.”
For the way forward, WHO is working in partnership with Ministries of Health, communities, Gavi, UNICEF, UNFPA and other partners to help increase availability and uptake of the vaccine for girls like Modesta, in the hope of saving many more lives to come.
Cancer of the cervix is the fourth most common cancer affecting women worldwide - and the second most common in lower-income regions. It is the only cancer that is almost entirely preventable through a safe, effective vaccine and screenings.
