Disease burden from seasonal influenza

A laboratory technician at work in the National Reference Laboratory in Dushanbe, Tajikistan, on 4 October 2023
Credit: WHO / Lindsay Mackenzie
Influenza, or the flu, is both a seasonal and a pandemic virus. Every year, mainly during the winter season, seasonal influenza infects as many as 1 billion people. This makes it one of the most common infectious respiratory viruses, after the common cold. Thankfully, the WHO Global Influenza Surveillance and Response System, or GISRS, monitors what viruses are circulating and twice a year recommends which viruses to target in the flu vaccine for the upcoming season. The flu vaccine is the best way to prevent infection and may reduce symptoms if you do get the flu. For those who are more vulnerable to flu, what we call ‘high risk groups’, the vaccine can save your life. Good hygiene practices can also reduce the risk of infection (for more information, see the factsheet here). Thankfully, although there are hundreds of millions of cases every year, the vast majority of these are not serious. Nevertheless, WHO estimates that there are 3 to 5 million cases of severe illness and between 290 000 to 650 000 respiratory deaths annually.
Disease burden from pandemic influenza

The awful effects of avian influenza
Credit: Scott Haugen
On the other hand, pandemic influenza follows when a new virus is transmitted to humans from another animal and spreads. Unfortunately, the fact that influenza viruses are found in birds, pigs and other animals in the wild is why we cannot eradicate influenza (unlike, for example smallpox that is only found in humans and WHO was able to eradicate in the 1960s and 1970s thanks to a highly effective vaccine amongst other factors). There will always be what are known as animal hosts. Most often animal-to-human (or zoonotic) infections cause sporadic or isolated infections in people, but not always. The WHO Global Influenza Programme has published a six-phase description of the pandemic process, from no infections in humans to sustained community outbreaks in two or more WHO Regions. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused a pandemic similar to influenza viruses that caused pandemics in the past, and influenza viruses will most likely be the cause of future pandemics. Here we look at the past four influenza pandemics, which, in total, caused almost 60 million deaths.
1918: Great Flu Pandemic

Emergency hospital during influenza epidemic, Camp Funston, Kansas (1918)
Credit: National Museum of Health and Medicine
As we don our poppies and pay our respects on Remembrance Day or Veterans Day every year in November, to mark the end of the First World War, we should also remember those who fell due to the influenza pandemic just after the war. In fact, more people died due to the influenza pandemic after the war (50 million) than died as a result of the war (17 million). Caused by the A(H1N1) virus, the intensity and speed with which the pandemic struck were almost unimaginable – infecting one-third (around 500 million people) of the Earth’s population at the time. It is believed that the virus was an avian virus passed on to humans from pigs.
1957-1958: Asian Flu
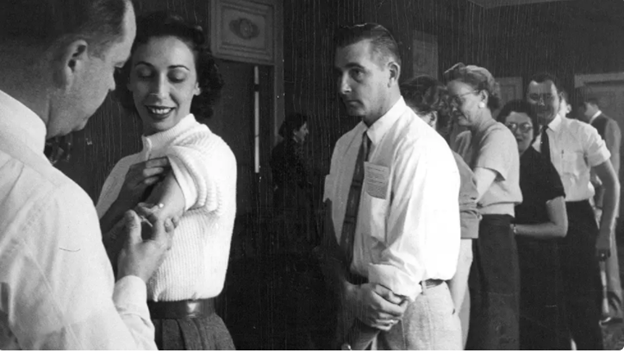
Denver Post employees get flu shots in November 1957
Credit: Dean Conger / The Denver Post via Getty Images
Between 1957 and 1958, an estimated one to four million people around the world died in an outbreak caused by the A(H2N2) virus. The virus was a combination of a virus of avian origin, probably from geese, and a human influenza virus. The pandemic started in Guizhou in southern China, but spread globally. The initial outbreak was reported in February, spread to Hong Kong SAR and Singapore by April, and across south-east Asia by the end of May. By June it had reached the United Kingdom and the United States of America. The race was on to prepare the vaccine before the northern hemisphere flu season in October. A vaccine was prepared and this, combined with improved health care and the availability of antibiotics against opportunistic bacterial infections, saved hundreds of thousands – if not millions - of lives.
1968-1969: Hong Kong Flu

Scores of patients crowd the waiting hall of a clinic on Hong Kong Island during the influenza epidemic in July 1968
Credit: SCMP
The A(H3N2) influenza virus that caused the Hong Kong flu pandemic 10 years later was descended from the A(H2N2) influenza virus that caused the Asian Flu pandemic. The outbreak followed a similar spread. It reached the UK in August and in the rest of Europe, India, and Australia in September. United States troops returning from Vietnam brought back the virus in September, but it didn’t spread widely until December. Those who got sick often missed work, which even affected post and rail services in the UK. In the US, President Johnson was hospitalized with flu-like symptoms, and President-elect Nixon got the flu. Although it only took 2 months to create the vaccine after receipt of the first vaccine strain, influenza cases had largely peaked before the vaccine could be administered widely. The pandemic caused an estimated one to four million deaths. Unlike in the US, in Japan, Europe, and Australia the flu season the following year caused even more deaths. The H3N2 virus is still in circulation today as one of the viruses causing seasonal flu.
2009-2010: Swine Flu

Nasal swabs from pigs in China to detect avian-like influenza virus
Credit: Honglei Sun
The 2009 “Swine flu” A(H1N1) pandemic started in Mexico in early 2009 and spread rapidly to over 200 countries and overseas territories or communities. Between 105 000 and 395 000 people are thought to have died. The virus was a new strain of H1N1 virus, the same virus that led to the 1918 Great Flu pandemic and the 1977 Russian flu outbreak. Although called swine flu, the virus is actually a combination of avian, swine, and human flu viruses further combined with a Eurasian pig flu virus.
2024 and beyond: Preparing for the next pandemic

Having a better understanding of the burden of influenza disease, including estimates of mortality and morbidity, supports informed decision-making on health policy and resource allocation. This applies to both annual seasonal influenza and to pandemic influenza viruses. Burden of disease estimates are crucial for strengthening national and global preparedness, prevention and control efforts. For example, they can inform governments and vaccine manufacturers of the quantities of vaccine and other medical products needed, and of the potential health, social, political, environmental and economic impacts of the disease on the individual and society.
As mentioned, WHO tracks seasonal influenza viruses and makes recommendations for vaccines through a large global network called GISRS. This network also monitors any other influenza viruses that could become pandemic viruses. It therefore acts as an alert mechanism. GISRS also strengthens laboratory surveillance to prepare for and respond to outbreaks. This network is planning to expand to other respiratory viruses of pandemic potential such as Respiratory Syncytial Virus (a disease that is very dangerous for babies), SARS-CoV-2 (the virus that causes COVID-19), and other potential viruses that pose an epidemic and pandemic threat.

Working alongside GISRS, the WHO Pandemic Influenza Preparedness (PIP) Framework brings together stakeholders to implement a global approach to pandemic influenza preparedness and response. It has, for example, signed agreements that have secured 10% of vaccine production (over 400 million doses) in the event of a pandemic.
You can protect yourself from seasonal influenza by being vaccinated and practicing good hygiene, while WHO supports countries to prepare for, detect, and rapidly respond to the next pandemic virus.
