Vaccines are one of the great public health achievements of the 20th century, but millions around the globe do not benefit from these medical interventions that can prevent serious disease and death.
While the pandemic has highlighted the lifesaving capabilities of vaccines and drawn more attention than ever to how vaccines are made and delivered, there continues to be a range of reasons why vaccination uptake is still so unequally distributed.
To enable programmes and partners to gather local data on the underlying causes behind low uptake, WHO has published its first ever position paper on behavioural and social drivers (BeSD). This represents a major milestone, as it brings the latest evidence and expertise to light, establishes new conceptions of the main drivers, and helps decision-makers and policy-makers to gain new insight on the most effective way to respond.
The paper established a new framework on BeSD of vaccination with 4 domains: thinking and feeling, social processes, motivation, and practical issues, including the experiences people have when trying to get vaccinated (Figure 1). The paper highlights the lesser-known factors that contribute to low uptake and the broad range of interventions necessary to counteract them. It also offers an updated definition of hesitancy as a motivational state of being conflicted above, or opposed to, getting vaccinated.
Figure 1. Behavioural and social drivers of vaccination framework
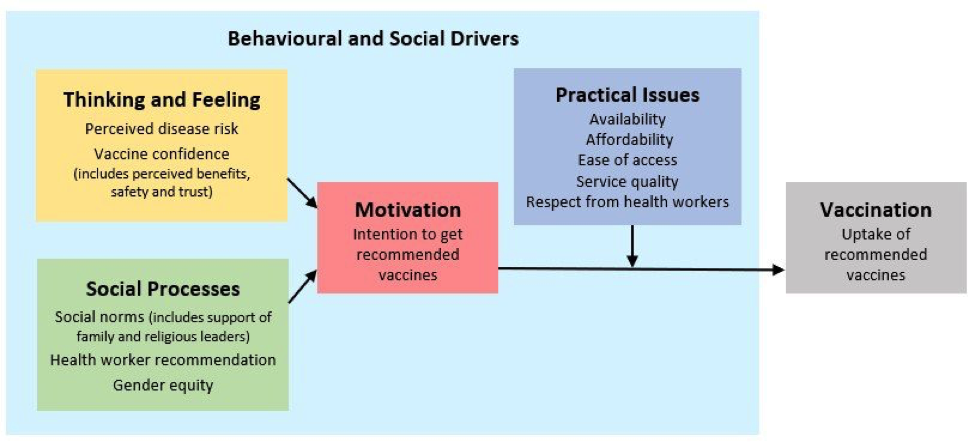
Source: The BeSD working group. Based on Brewer et al. Psychol Sci Public Interest. (2017).
But it is not enough to gather data to better diagnose reasons for low uptake. To help programmes to move from understanding BeSD to acting on them, the paper elaborates on effective interventions to increase vaccination.
Factors that increase uptake, when supported by political commitment, a strong health workforce, local data, include:
- Quality services that offer convenience, efficiency, respectful experience, negligible out-of-pocket costs
- Engagement of trusted figures, such as community representatives or advocates
- Tailored communications and education, particularly through dialogue-based interventions such as 1:1 counseling with a trusted nurse or doctor
- Supportive policies, including SMS reminders, default appointments, tailored incentives, onsite vaccination services
The position paper finishes with recommendations that countries regularly collect standardized data using BeSD validated surveys and priority indicators, focusing on districts and populations with coverage gaps and inequities. To complement this data, BeSD interview guides may be used for prioritized populations to ensure an in-depth understanding of beliefs and experiences.
Until now, the lack of clarity around current issues, including those inhibiting COVID-19 vaccine uptake as well as routine immunizations, has left many national public health officials grasping for answers. By introducing this critical insight and these useful tools, we make an important step towards global health for every citizen.
To read the position paper and gain access to these new, innovative tools, download the article here.
- Understanding the behavioural and social drivers of vaccine uptake. WHO position paper – May 2022
- Behavioural and social drivers of vaccine uptake: tools and practical guidance
