Oxygen
10 October 2024 | Questions and answers
Oxygen (O2) is a chemical element. At standard temperature and pressure, two oxygen atoms bind together to form a colourless and odourless gas with a molecular mass of 32 atomic mass units (amu). Together with nitrogen and argon, oxygen is one of the three major constituents of Earth’s atmosphere, being present in 21% of air.
Medicinal oxygen is an essential medicine with no substitution. Medicinal oxygen composition is established in the pharmacopeias, such as the International Pharmacopeia. Healthcare professionals use it to treat respiratory diseases like COVID-19 and pneumonia. It is administered to patients as an inhalation gas. Medicinal oxygen differs from industrial oxygen in that medicinal oxygen is tested to meet authorized specifications for its identity, purity and content by following Good Manufacturing Practices (GMP) and Good Storage and Distribution Practices (GSDP) established in the regulatory framework for medicinal gases.
The oxygen ecosystem refers to holistic efforts, initiatives and resources across health systems, that are required for an optimal and sustainable implementation of oxygen systems. In addition to equipment and the medicine itself, the oxygen ecosystem also covers all of the other activities to ensure that oxygen systems can function safely, effectively and continuously. The ecosystem considers context, policies, guidelines, need-gap assessments, health infrastructure, the selection of appropriate systems, costing and financing, partnerships, implementation, operation and maintenance, training, monitoring and evaluation. And sustaining oxygen ecosystems means revisiting all of these aspects at a set frequency.

The oxygen systems for medical use include, but are not limited to, oxygen source (or production), storage, distribution and delivery supplies, as well as various items for flow regulation, conditioning, quality assurance (QA), quality control (QC) and safety. The long-term sustainability of oxygen systems requires a holistic approach, and a resource ecosystem focused not only on oxygen production but also on distribution and delivery, ongoing maintenance and upkeep.
Medicinal oxygen can be produced by air liquefaction process or by pressure swing adsorption, vacuum swing adsorption or combined vacuum pressure swing adsorption technology.
Depending on the source and production method the medical oxygen has the following characteristics:
- By the air-liquefaction process – according to the International Pharmacopoeia and to the Revision of the monograph on Oxygen for inclusion in The International Pharmacopoeia (October 2021), medicinal oxygen produced by air-liquefaction must contain not less than 99.5% v/v of O2. Cryogenically produced liquid oxygen is always generated off-site (not at a medical facility).
- By Pressure Swing Adsorption (PSA) plants and Vacuum Swing Adsorption (VSA) plants – according to the Revision of the monograph on Oxygen for inclusion in The International Pharmacopoeia (October 2021) and to WHO interim guidance technical specifications for PSA plants (June 2020) pressure swing adsorption technology produces medical oxygen with 93±3 % O2 from ambient air. By bedside oxygen concentrators – according to WHO-UNICEF technical specifications and guidance for oxygen therapy devices (2019) and WHO interim guidance of WHO list of Priority Medical devices for COVID-19 and its associated technical specifications (2020), stationary bedside oxygen concentrators are those which deliver low-flow, continuous, clean oxygen (more than 82 %). It is a self-contained, electrically powered medical device designed to concentrate oxygen from ambient air using a pressure swing adsorption process. Oxygen concentrators have typically wheels to be moved between clinical areas; likewise are more frequently used for home oxygen therapy. Each concentrator can cover one or more patients if using appropriate flowsplitters. As any other medical device, proper maintenance and infection prevention and control measures should be considered.
Further information can be found in Chapter 2. Health facility oxygen systems of Foundations of medical oxygen systems (who.int)
Oxygen is produced from air liquefaction, Pressure Swing Adsorption (PSA), or Vacuum Swing Adsorption (VSA) technology. After this, depending on the source, it may be stored, delivered to patients, or transported to a final offsite destination.
Liquid oxygen will always first be stored. When converted from liquid to gas, it can travel through pipes to patients (through a medical gas distribution system, MGPS), or compressed to fill high-pressure gas cylinders.
Oxygen generation plants such as Pressure Swing Adsorption (PSA), Vacuum Swing Adsorption (VSA) and Vacuum Pressure Swing Adsorption (VPSA) can produce oxygen for immediate delivery to patients (through a medical gas distribution system), or to fill cylinders for storage or transport. Cylinders must always be handled by trained personnel as the contents are under extreme pressure.
Oxygen sources and distribution for COVID-19 treatment centres- https://www.who.int/publications/i/item/oxygen-sources-and-distribution-for-covid-19-treatment-centres.
Oxygen Access Scale Up- https://www.who.int/initiatives/oxygen-access-scale-up
Oxygen is carried from the lungs around the body in haemoglobin in red blood cells. When leaving the lungs, the red blood cells are normally carrying close to the maximum oxygen then can; the “oxygen saturation” is high. It is normal for the oxygen to leave the red blood cells after they pass through the capillaries in the body’s organs. The oxygen saturation falls and the “desaturated” red blood cells then return to the lungs to be refilled. When oxygenated blood first arrives in the organs the oxygen saturation should be high. If the oxygen saturation is low at this point (known as hypoxemia) it can lead to an oxygen shortage in organs such as the brain, heart, and kidneys. This affects their function, and at worst can lead to organ failure. Low oxygen saturation occurs in many diseases, particularly those affecting the lungs. Supplemental (“extra”) oxygen is essential for treating this hypoxaemia to bring the blood oxygen level up, and keep the organs functioning.
Oxygen saturation is measured as a percentage, with levels of 94% or more being normal.
Technical specifications for oxygen concentrators- https://www.who.int/publications/i/item/9789241516914
WHO’s Science in 5 on COVID-19: Medicinal oxygen- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-33---medical-oxygen
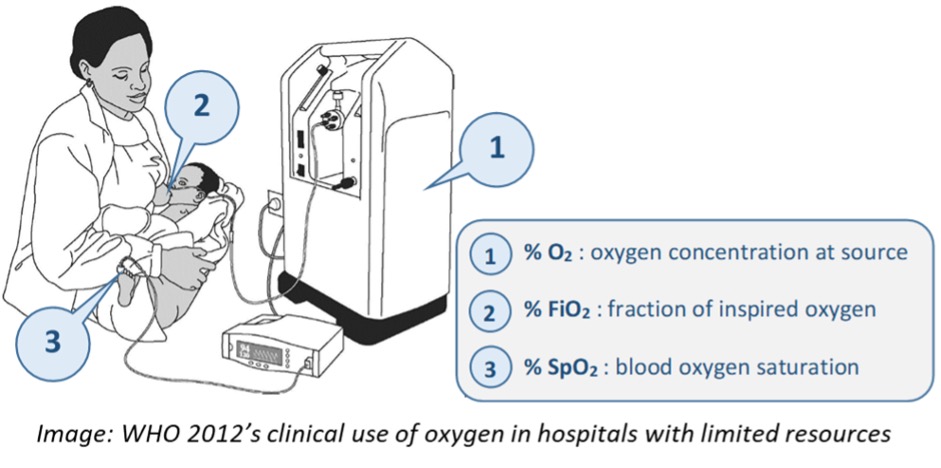
Oxygen saturation is usually measured in the arteries, or in the smaller blood vessels (arterioles and capillaries). Measuring arterial blood oxygen requires a needle to remove a sample, usually from the wrist, and a blood gas analysis machine and reagents. While it can give a very accurate measurement, it is invasive, sometimes difficult, and relatively expensive. The measurement is called the SaO2.
We can measure oxygen saturation in the very small arterioles and capillaries using a pulse oximeter. It is not invasive, requires relatively cheap equipment, and no reagents are necessary. This method shines a light from one side of the patient’s finger, toe or earlobe, and measures the light reaching a sensor on the other side. By comparing two different wavelengths of light, the pulse oximeter can sense the oxygen saturation. This is because oxygenated and deoxygenated blood absorb the light differently. The measurement is called the SpO2.
When assessing a patient, pulse oximetry is a foundation of good medical practice. It is often referred to as the fifth vital sign. Medical practitioners must know the functions and limitations of pulse oximetry and have a basic knowledge of oxygen saturation.
Oxygen therapy for children- https://www.who.int/publications/i/item/9789241549554
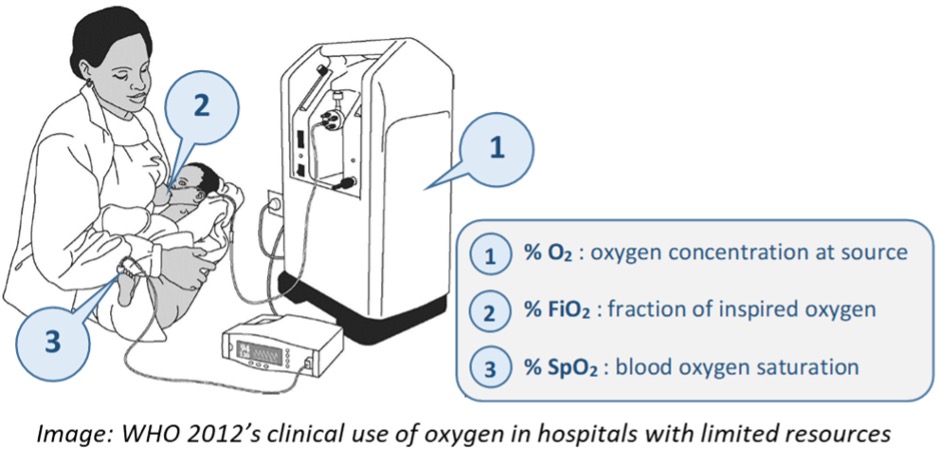
Pulse oximetry is the most accurate non-invasive method for detecting hypoxaemia. Pulse oximeters are reliable and now available at low cost. By detecting and monitoring hypoxaemia, it can help us make more efficient use of oxygen supplies and improve patient safety – a pulse oximeter is an essential medical device.
It measures the percentage of oxygenated haemoglobin (SpO2). The pulse oximeter consists of a light source, a sensor, and an electronic chip to calculate, and a screen to display the results. In addition to the oxygen saturation and the pulse rate, many models also show a representation of the pulse wave (plethysmography).
After the probe is clipped to the finger, toe or earlobe, it can give a result in seconds.
Priority medical devices list for the COVID-19 response and associated technical specifications- https://www.who.int/publications/i/item/WHO-2019-nCoV-MedDev-TS-O2T.V2
WHO-UNICEF Technical specifications and guidance for oxygen therapy devices- https://www.who.int/publications/i/item/9789241516914
Oxygen therapy for children- https://www.who.int/publications/i/item/9789241549554
The average SpO2 at sea level is around 97–99%, with a lower limit (mean minus 2 standard deviations) of 94%. Normal oxygen saturation values fall as you go higher .
Oxygen therapy for children- https://www.who.int/publications/i/item/9789241549554
Oxygen therapy involves giving patients extra (“supplemental”) medical oxygen through a mask or similar device. Decisions about when to give oxygen therapy must be overseen by trained clinical staff, and include proper monitoring. Pulse oximeters are an important low-cost technology and the accepted standard for detecting hypoxaemia, and for monitoring oxygen therapy. When combined with an properly regulated oxygen supply, pulse oximetry can support the efficient use of oxygen.
Oxygen therapy is a highly effective intervention for reducing deaths. WHO guidelines emphasize the importance of oxygen and its broad indications for neonates, paediatrics, obstetrics, internal medicine, emergency care, triage, anaesthesia, surgery, trauma, survival services, and pandemic preparedness and treatment of other common medical conditions and illnesses affecting patients of all ages.
Oxygen sources and distribution for COVID-19 treatment centres- https://www.who.int/publications/i/item/oxygen-sources-and-distribution-for-covid-19-treatment-centres
The methods used to give oxygen to patients should be safe, simple, effective and inexpensive. The most common is non-invasive, delivered through a face mask, or tube positioned at the tip of the nostril. Semi-invasive devices include nasopharyngeal catheters which are slightly longer tubes passed into nose and back of the throat. Semi-invasive delivery methods require a low oxygen flow and are cheaper than non-invasive methods, which require higher oxygen flows. Other forms include masks which can cover the mouth and nose, held with elastic straps around the back of the head.
Nasal prongs are often preferred, especially in children, because they balance efficiency and patient comfort. If more oxygen is required, masks and other devices may be used.
Oxygen therapy for children- https://www.who.int/publications/i/item/9789241549554
Oxygen sources and distribution for COVID-19 treatment centres- https://www.who.int/publications/i/item/oxygen-sources-and-distribution-for-covid-19-treatment-centres
COVID-19 Clinical management: living guidance- https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1
Very high levels of supplemental medical oxygen for prolonged periods can be harmful, particularly in prematurely-born or low birth-weight babies.
WHO guidelines emphasise the careful monitoring of oxygen therapy to prevent such risks. Oxygen should be administered and monitored based on clinical guidelines to avoid lung and other organ damage. Guidelines based on the rational use of oxygen.
For all patients, but especially neonates, it is important that healthcare providers are trained to administer the right amount of oxygen using the right device for the right length of time.
Oxygen therapy is usually given continuously, including overnight, until a patient has stabilized at a normal SpO2. Healthcare providers should consider which delivery interface may be most comfortable to not disrupt a patient in their sleep.
Related
- Oxygen sources and distribution for COVID-19 treatment centres
- Oxygen Access Scale Up
- Technical specifications for oxygen concentrators
- WHO’s Science in 5 on COVID-19: Medicinal oxygen
- Oxygen therapy for children
- Priority medical devices list for the COVID-19 response and associated technical specifications
- WHO-UNICEF Technical specifications and guidance for oxygen therapy devices
- COVID-19 Clinical management: living guidance
- Home care for patients with suspected or confirmed COVID-19 and management of their contacts
