Sepsis is the most common serious complication of infection. It affects people worldwide, but has a particularly high burden in low- and middle-income countries where resources to treat it are more limited. Estimates from 2017 suggest 48.9 million cases of sepsis occur each year, with 11 million deaths. Many people who survive sepsis suffer long-term complications as a result.1
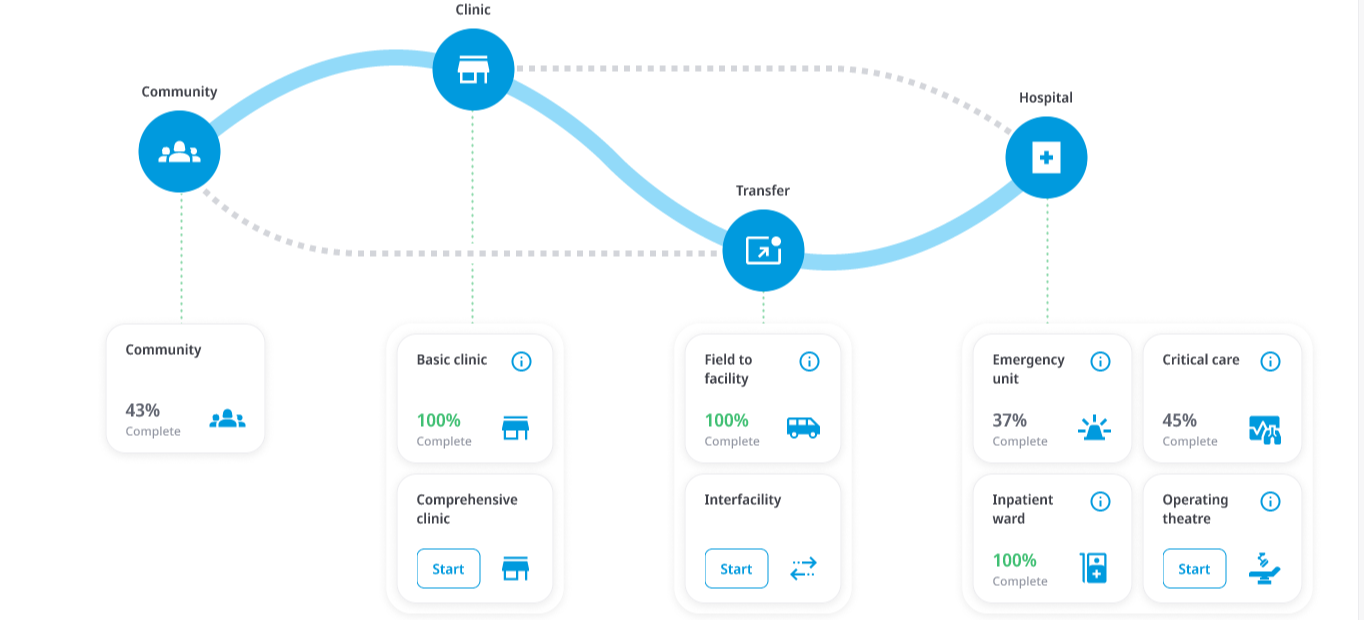
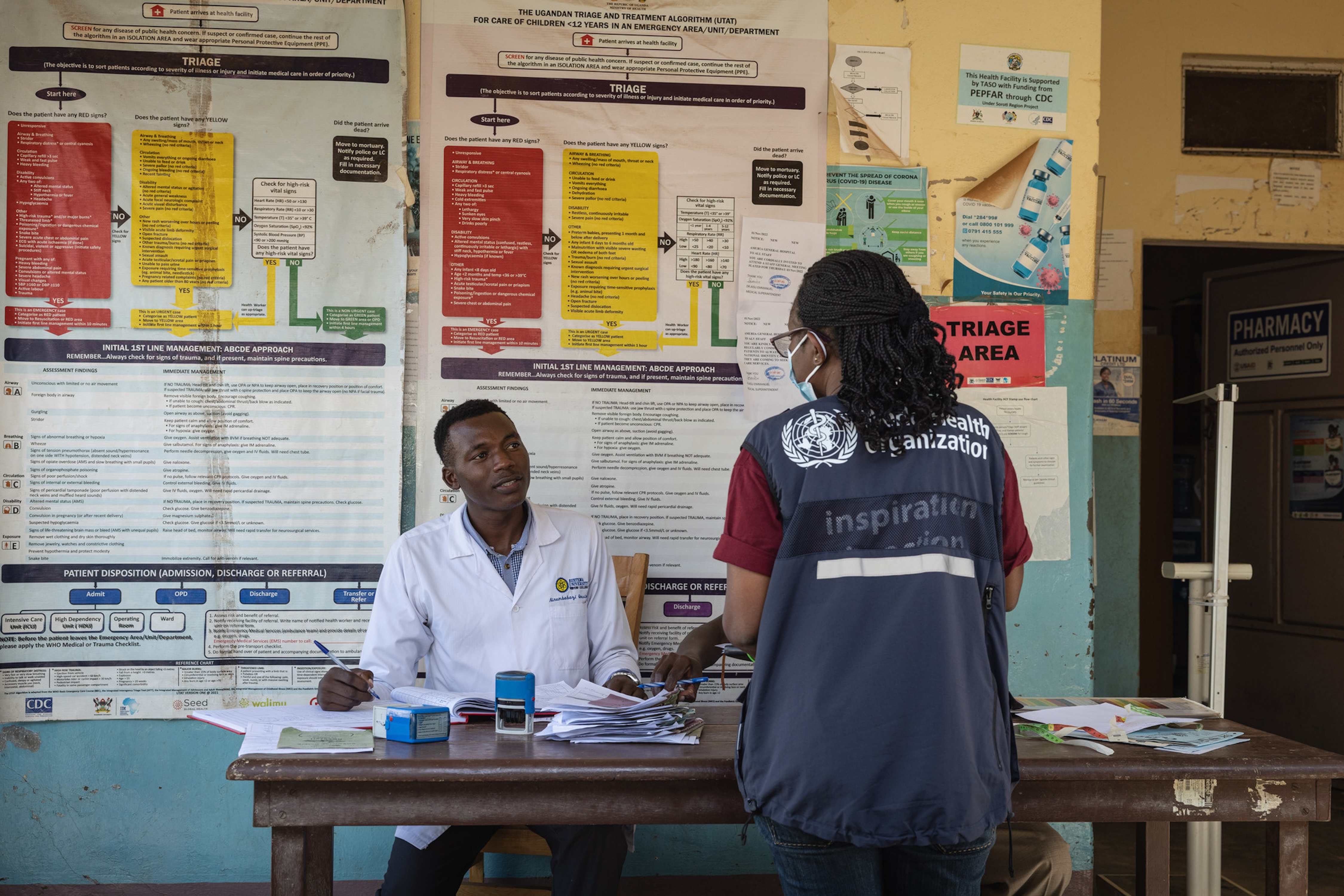
Treatment for sepsis can save lives. Treatment requires quality integrated clinical care with primary care linked to emergency, critical and operative care by communication, transportation, referral and counter-referral mechanisms.
The 70th World Health Assembly called for the development of guidance on sepsis prevention and management to support Members States in “Improving the prevention, diagnosis and clinical management of sepsis” [WHA resolution 70.7].2
To improve clinical outcomes, people with sepsis require effective systems of care, which include key functions such as early recognition, resuscitation, targeted antimicrobial therapy, source control, intensive monitoring and detection of clinical deterioration, and continuing prevention of organ failure and complications. Effective and efficient critical care and early operative care can further reduce mortality and morbidity in health settings globally.