Prehospital toolkit
Overview
Timely care and rapid transport save lives, reduce disability and improve long term outcomes. Prehospital emergency care is a key component of the health care system. Strengthening prehospital care can help address a wide range of conditions across the life course, including injury, complications of pregnancy, exacerbations of non-communicable diseases, acute infections and sepsis. The prompt provision of care and rapid transport from the scene to a facility can save lives, reduce disability and improve long-term outcomes.
The primary purpose of prehospital emergency care is to provide rapid assessment, immediate management and transportation of patients to appropriate medical facilities. Strengthening health systems to deliver effective prehospital care - including linkages from communities to facilities and between facilities - is essential to meeting people’s health needs across the life course and is essential to a primary health care centred approach and making progress towards Universal Health Coverage.
Despite their proven potential to reduce disability and save lives, prehospital systems are often underdeveloped. Many health systems lack an enabling regulatory framework, coordination mechanisms, trained personnel, and adequate equipment and infrastructure, leading to delayed or inadequate emergency care and poor outcomes. Establishing standard operational frameworks and protocols enhances the effectiveness of prehospital care, helping ensure that all individuals have access to timely, quality emergency care, regardless of their location.
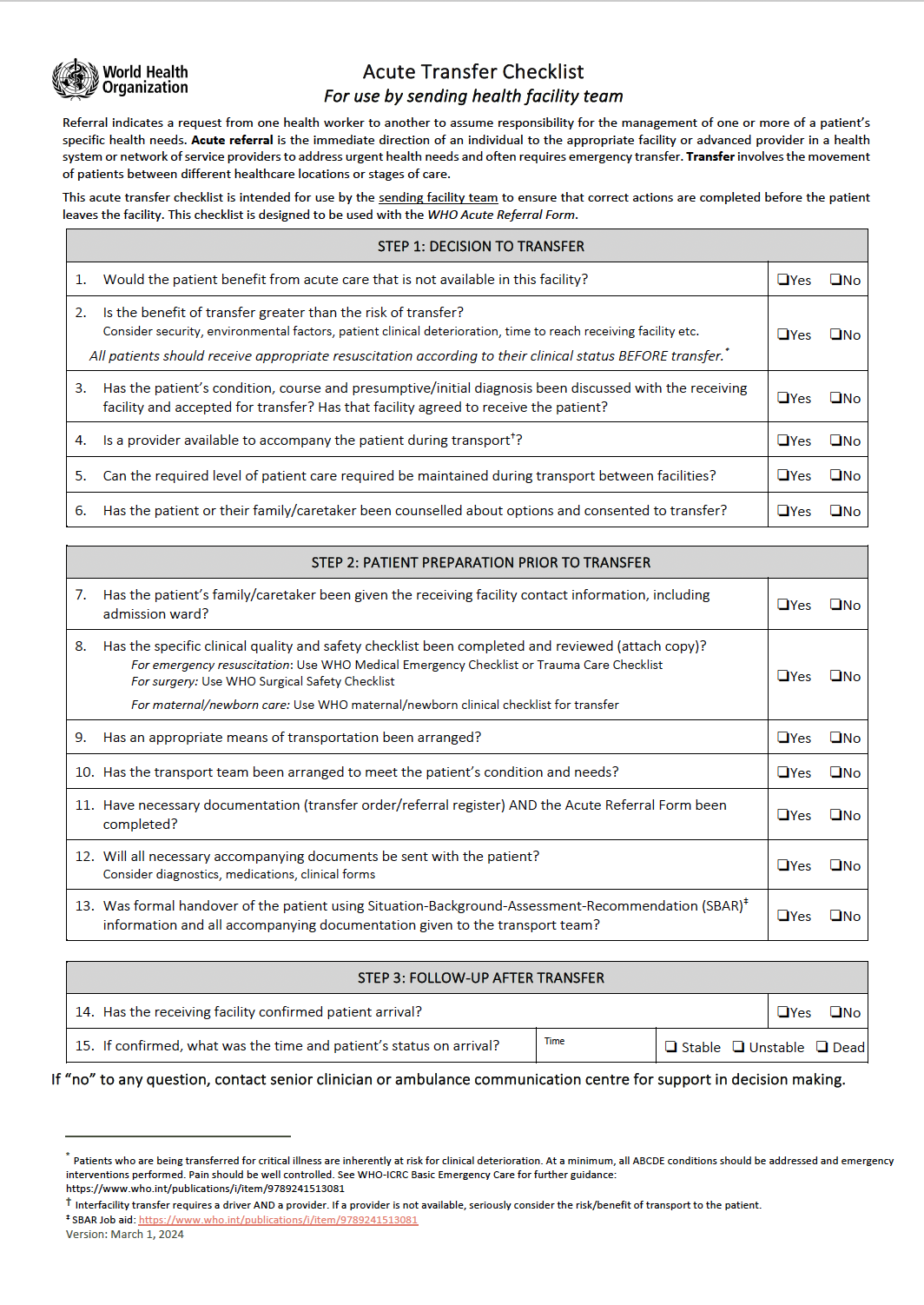
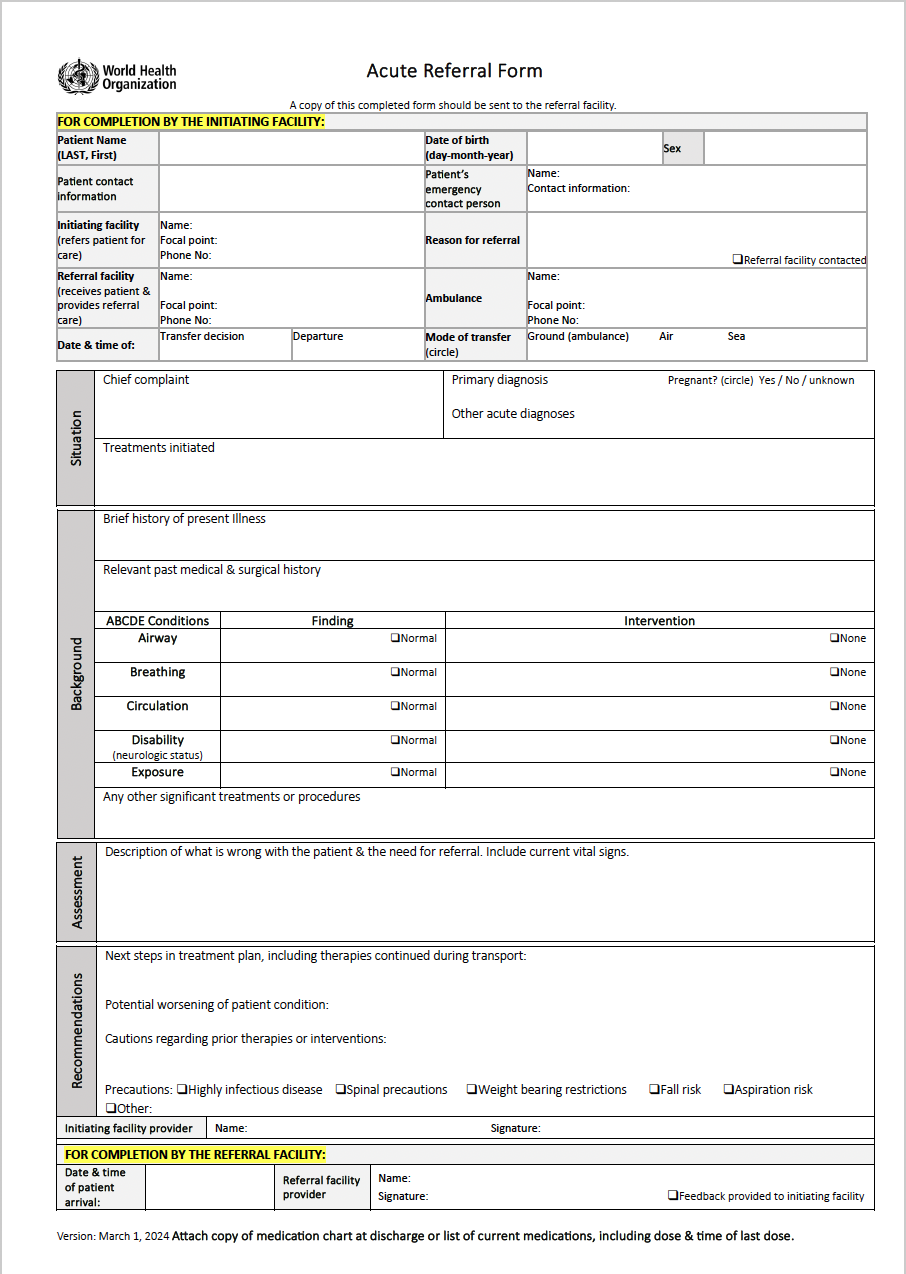
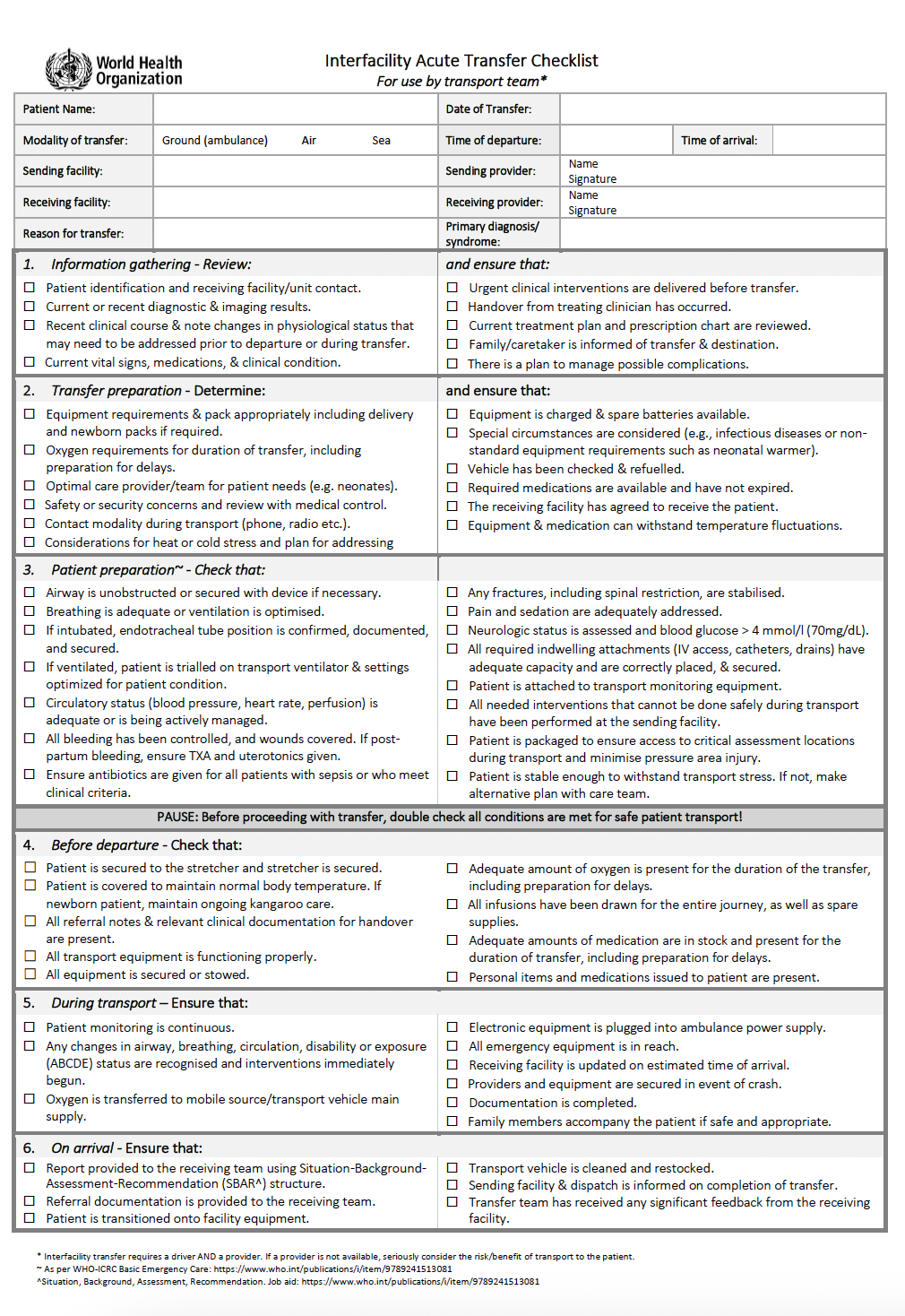
WHO’s prehospital toolkit is a bundle of products designed to help strengthen prehospital emergency care systems. These tools are intended to help address commonly identified gaps in the main components of a prehospital system (governance, operations, prehospital provider training, equipment & medication, communication and quality improvement). They can be used to support the development of prehospital services in all resource settings.
Related links
Health topics
Contact us