As many countries and areas are easing public health and social measures, governments, businesses, communities and individuals all play important roles in managing COVID-19. This reflects a move from an acute pandemic response towards a sustained management approach, which aims to reduce the risk of serious illness, minimize deaths and protect health systems, while supporting ongoing social and economic recovery.
Now more than ever, all levels of society have specific roles to play, contributing to the broader goal of protecting people from COVID-19 in the longer term. WHO Regional Director for the Western Pacific, Dr Takeshi Kasai said, “When population-based measures are eased, it does not mean countries are giving up on controlling COVID-19. Rather, governments and people will need to move to an approach that sustainably manages COVID-19 in the future.”
The sustained management approach for COVID-19 in the Western Pacific Region includes five key elements: vaccination, public health and social measures appropriately calibrated for the local context, protecting the health system, early detection and targeted response, and international border measures (again, appropriately calibrated for the context). These should be supported by strong surveillance, contact tracing and monitoring, and clear communication.
“Now, governments need to reach every vulnerable person with vaccines, refine surveillance for effective decision-making, ensure health systems are arranged in a way to provide services to those who need them. We must also clearly communicate with businesses, communities and individuals about what they need to know, so they can take the most appropriate action.” Read Dr Kasai’s remarks on sustained management of COVID-19.
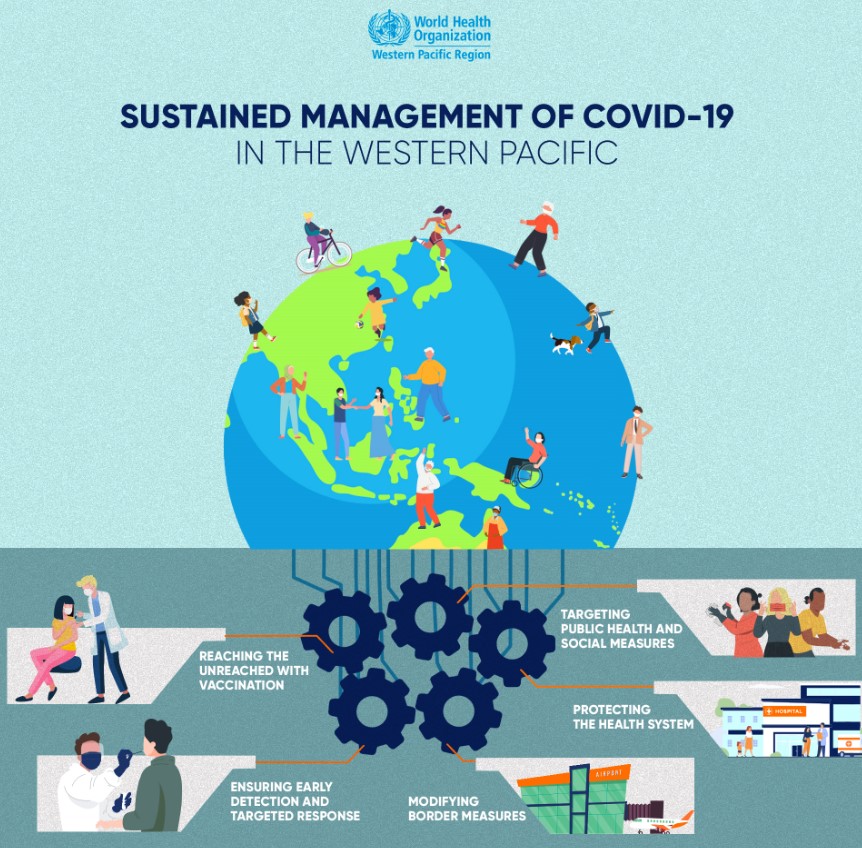
Reaching the unreached with vaccination
With high vaccination coverage of health-care workers across the Region, the focus must be on efforts to vaccinate every older person, every person with an underlying health condition, and everyone with a higher risk of infection or more difficulty in accessing health services. This may include people living in remote or hard-to-access parts of a country.
“We cannot think of ourselves as separate from others. One person who is not vaccinated or one person who has no access to health services represents an equity issue for our society. We can’t just talk about our own vaccination; we must ensure that others are vaccinated as well. Our own protection relies on other people’s protection,” said Dr Dulce Natividad, Associate Professor at the University of the Philippines during a vaccination drive in Manila for people experiencing homeless and survivors of gender-based violence.
Targeting public health and social measures
Public health and social measures need continual adjustment, depending on the evolving local situation, to decrease transmission of the virus without causing major social or economic disruption.
Individuals should take measures when and where appropriate. These include: keeping a safe distance from others, avoiding crowds and places that are not well ventilated, wearing a well-fitted mask covering the mouth and nose, cleaning hands regularly, and covering coughs and sneezes. Situations calling for these measures include: when there is a surge in COVID-19 cases; when you are in closed, confined spaces; or when visiting older adults or people with underlying health conditions. People need to know when to scale up these measures. For example, during Ramadan festivities in Malaysia, WHO advised people on ways to be proactive and smart to protect themselves and those around them. People should also be vaccinated against COVID-19.
Decision-makers who are responsible for workplaces, businesses, events and other gatherings need to take actions to keep settings safe, such as ensuring policies are in place to encourage physical distancing in markets, improving ventilation in factories and organizing events outdoors.
In the Lao People’s Democratic Republic, children have been able to keep learning thanks to a Safely Back to School campaign, which included multisectoral collaboration and community engagement, clear communication, and measures including masks, distancing, ventilation, cleaning and a “stay home when sick” policy.
Protecting the health system
Governments may choose to adopt population-based measures such as lockdowns, if there is widespread transmission of COVID-19 and low vaccination coverage, and a risk of crossing the “red line” where health systems are overwhelmed. But, in the long term, these measures will be exceptional. Instead, governments can rapidly calibrate a range of measures (which fall short of lockdowns – for example, compulsory masks in indoor venues) as needed, to minimize deaths and protect the health system’s ability to meet all community needs, not just those of people with COVID-19.
To protect health systems and reduce pressure on health-care workers, people who test positive but have no symptoms or only mild illness should isolate and recover at home. This saves hospital beds for people who are more seriously ill, whether it is COVID-19 or other illness.
To help governments make the most effective use of their health systems, WHO in the Western Pacific Region has published technical advice on various topics:
• the care of older people and people living in long-term care facilities, other non-acute care facilities and home care;
• the role of primary health care;
• managing hospital services, including maintaining essential routine health care and generating surge capacity;
• implementing telemedicine services during COVID-19; and
• actions to consider in the care and protection of vulnerable population groups.
Ensuring early detection and targeted response
While diagnosing and counting every case, tracing every contact, or carrying out mass testing may no longer be necessary, it will remain important to detect cases and clusters early, especially among vulnerable populations, such as people who are older, have underlying health conditions or are at higher risk of severe infection.
Countries should ensure they have good systems for detecting cases in settings such as health-care facilities and care homes for older people, as well as among vulnerable communities, such as people living in overcrowded housing, refugees and migrants, people with disabilities, people living in poverty and people experiencing homelessness. Read the updated WHO Western Pacific Region guidance on surveillance of vulnerable populations.
Modifying border measures
Governments have successfully implemented border measures to delay the introduction of COVID-19 and variants of concern into some countries and areas, while they prepared their health systems, rolled out and accelerated COVID-19 vaccination.
This was the case in Cambodia, where risk-based measures were used at its international borders to delay the arrival of the Omicron variant to further strengthen the country’s public health and health-care system.
With the virus expected to continue circulating for some time and many borders now fully open, all countries should expect further cases. Countries and areas should take measures to strengthen capacities for coordination and management of travellers at points of entry. Read the WHO Western Pacific Region guidance on taking a risk-based approach to border measures as local, regional and global travel returns.
Facing future challenges
As long as the virus is in circulation, governments, businesses, communities and individuals need to stay vigilant and use a combination of tools to limit its spread and its impact. If every part of society plays its role, appropriate to its context and specific setting, we can limit transmission, reduce the risk of the emergence of new and more dangerous variants, protect the most vulnerable and those at high risk, and allow people to return to living the lives that we all want.




