Inputs needed to support HBP design |
The resources in this section represent the inputs needed in terms of the financing and resource requirements as well as the evidence inputs, or data, that is needed for the Assessment phase of priority-setting.
Financing and Resources Requirements
Another critical element of developing an HBP process is establishing the appropriate financing and resource requirements. It has been pointed out that producing HTA’s are not cheap, with some estimates in the range of EUR 30,000 to EUR 100,000 per HTA study in EU country settings (MSH roadmap). Countries also have the option of conducting studies that are more limited than a full HTA study through processes such as RapidHTA, MiniHTA, Adaptive HTA, and others that are suitable for their purposes. While these may be less resource intensive, the limitation of these studies should be noted, and the use of them should be done within a reasoned framework. Countries will also need to consider how many studies will be required each year (or in the relevant time period), which will also mean having a clear understanding of whether there will be multiple full-package reviews, or ongoing incremental analyses. Studies can either be conducted in-house by a given agency, contracted out to academics or other research groups, or conducted by industry in order to satisfy the requirements of submission. In each case, appropriate resources need to be considered including having adequate capacity for independent evaluation of the studies.
UHC Compendium
When undertaking the task of developing packages of services, it is important to have a comprehensive list of services and interventions for reference. Assessing already existing packages is helpful, as is consulting other packages and scanning for interventions that may be missing or emerging at the time.
One tool for identifying the services to be considered for inclusion in a package is the UHC Compendium. A description of the Compendium, as provided on the website is given here:
The UHC Compendium is a database of health services and intersectoral interventions designed to assist countries in making progress towards Universal Health Coverage (UHC). It provides a strategic way to organize and present information and creates a framework to think about health services and health interventions. The database for the Compendium spans the full spectrum of promotive, preventive, diagnostic, resuscitative, curative, rehabilitative, and palliative services, as well as a full complement of intersectoral interventions. The Compendium will provide rapid one-stop access to supporting evidence, associated human and material resource inputs, and feedback on cost impact as interventions are selected.
In addition to listing the services and interventions to be considered, the UHC Compendium also provides valuable data that can be used to inform priority-setting and benefit package design, including human and material resource requirements as well as global cost-effectiveness estimates for the listed services1.
1. Human and material resource requirements and cost-effectiveness data are currently only available for a selection of services. That selection is being expanded over time with the goal of eventually covering the majority of the services.
UHC Service Package Delivery and Implementation (SPDI) Tool
Using the UHC Compendium data, the UHC Service Package Delivery & Implementation (SPDI) Tool supports countries to develop well-designed national health service packages. SPDI is a selection interface where users will access data from the global UHC Compendium database and select content for inclusion in their benefit package. It supports the design of more implementable packages that include health promotion and prevention, treatment, rehabilitation and palliative care services across the life course.
Global estimates of cost-effectiveness will also be available to guide benefit package selections in SPDI.
Links to other WHO databases and guidelines
The UHC Compendium provides one-stop access to WHO guidelines, classification systems, and associated human and material resource needs to support effective service delivery.
The UHC Compendium is a reference for country-specific workforce and education planning, and links directly to other key products for competency-based education outcomes and Workload Indicators of Staffing Need (WISN).
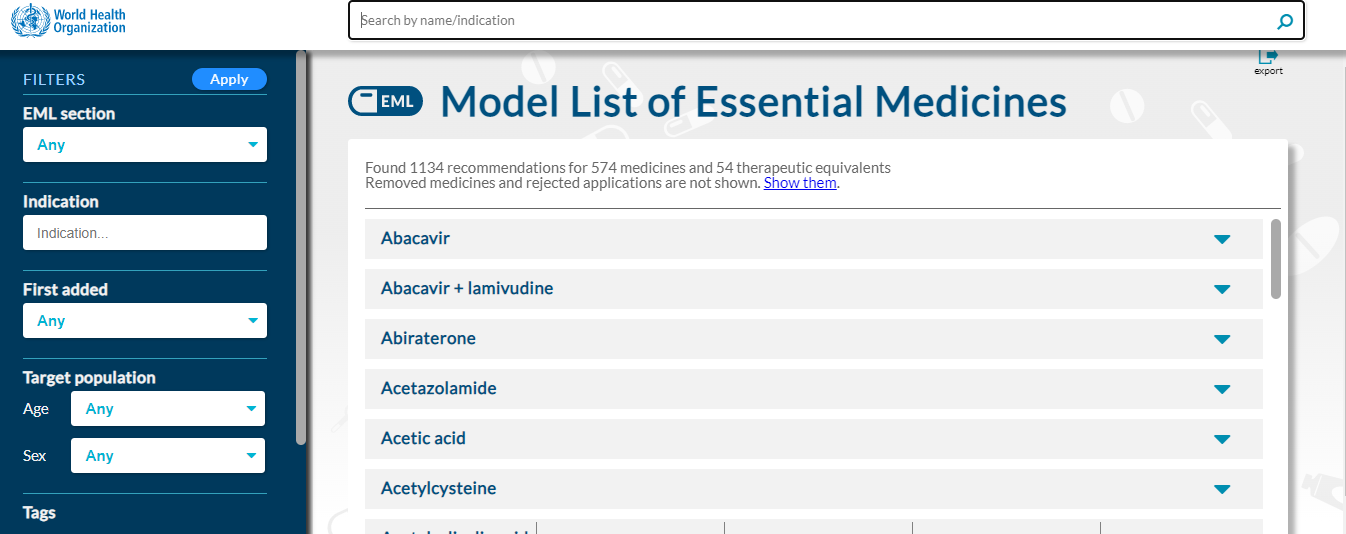
The Compendium also supports countries to link their service packages with existing material resource planning tools: Model List of Essential Medicines (EML), Model List of Essential In Vitro Diagnostics (EDL), Priority Assistive Products List (APL), and List of Priority Medical Devices (PMD).
Finally, the Compendium includes linkages to sustainable development goals (SDGs) and to common online tools for classifying diseases and services, including the international classification of disease (ICD-11), the international classification of health interventions (ICHI), and the international classification of functioning (ICF).
WHO-CHOICE
The WHO CHOosing Interventions that are Cost- Effective (CHOICE) project publishes and disseminates data on the cost-effectiveness of a wide range of health interventions at a regional-level. A standardized method of cost-effectiveness analysis is used, allowing comparability between interventions and simultaneous evaluation of new and existing interventions. The most recent WHO-CHOICE regional estimates are published in a series of papers, as described below.
| Resource | Description | Reference |
1. Methods for the Economic Evaluation of Health Care Interventions for Priority Setting in the Health System: An Update From WHO CHOICE | This paper provides an overview of the WHO-CHOICE methodology, focusing on updates made over the past 10 years, including on time horizon and discount rates. | Bertram MY, Lauer JA, Stenberg K, Edejer TTT. Methods for the economic evaluation of health care interventions for priority setting in the health system: an update from WHO CHOICE. Int J Health Policy Manag. 2021;10(11):673–677. doi:10.34172/ijhpm.2020.244 |
2. Cost-Effectiveness of Interventions to Improve Maternal, Newborn and Child Health Outcomes: A WHO-CHOICE Analysis for Eastern Sub-Saharan Africa and South-East Asia | This paper presents cost-effectiveness estimates for immunization, child health care, nutrition, reproductive health, and maternal/newborn health interventions.
| Stenberg K, Watts R, Bertram MY, Engesveen K, Maliqi B, Say L, Hutubessy R. Cost-effectiveness of interventions to improve maternal, newborn and child health outcomes: a WHO-CHOICE analysis for Eastern sub-Saharan Africa and South-East Asia.Int J Health Policy Manag. 2021;10(11):706–723. doi:10.34172/ijhpm.2021.07 |
3. Priority Setting in HIV, Tuberculosis, and Malaria – New Cost-Effectiveness Results From WHO-CHOICE | This paper presents cost-effectiveness estimates for HIV, tuberculosis and malaria prevention and treatment interventions. | Ralaidovy AH, Lauer JA, Pretorius C, Briët OJ, Patouillard E. Priority setting in HIV, tuberculosis, and malaria – New cost-effectiveness results from WHO-CHOICE. Int J Health Policy Manag. 2021;10(11):678–696. doi:10.34172/ijhpm.2020.251 |
4. Cost-Effectiveness of Population Level and Individual Level Interventions to Combat Non-communicable Disease in Eastern Sub-Saharan Africa and South East Asia: A WHO-CHOICE Analysis | This paper presents cost-effectiveness estimates for non-communicable disease and mental health prevention, promotion and management interventions. | Bertram MY, Chisholm D, Watts R, Waqanivalu T, Prasad V, Varghese C. Cost-effectiveness of population level and individual level interventions to combat non-communicable disease in Eastern sub-Saharan Africa and South East Asia: a WHO-CHOICE analysis. Int J Health Policy Manag. 2021;10(11):724–733. doi:10.34172/ijhpm.2021.37 |
5. Progressive Realisation of Universal Health Coverage in Low- and Middle-Income Countries: Beyond the “Best Buys” | This paper presents a cross-programme analysis of the comparative cost-effectiveness of 479 intervention scenarios across 20 disease programmes and risk factors. | Bertram MY, Lauer JA, Stenberg K, Ralaidovy AH, Edejer TTT. Progressive realisation of universal health coverage in low- and middle-income countries: beyond the “best buys.” Int J Health Policy Manag. 2021;10(11):697–705. doi:10.34172/ijhpm.2020.245 |
Furthermore, the most recent WHO-CHOICE cost-effectiveness estimates are mapped to the UHC Compendium in the cost-effectiveness section of the UHC Compendium website, as described above.
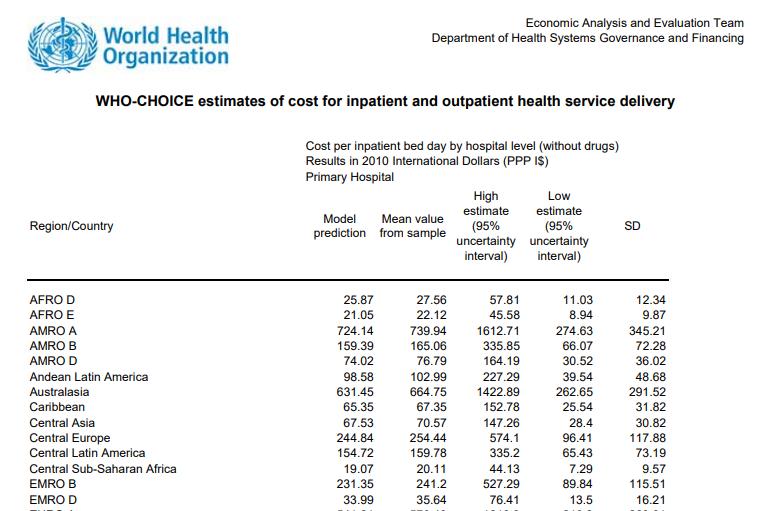
Unit Cost Database
WHO also maintains estimates of unit costs of service delivery at the country and regional levels. Costs per outpatient visit and costs per hospital bed-day are presented and include all cost components, with the exception of drugs and diagnostics.
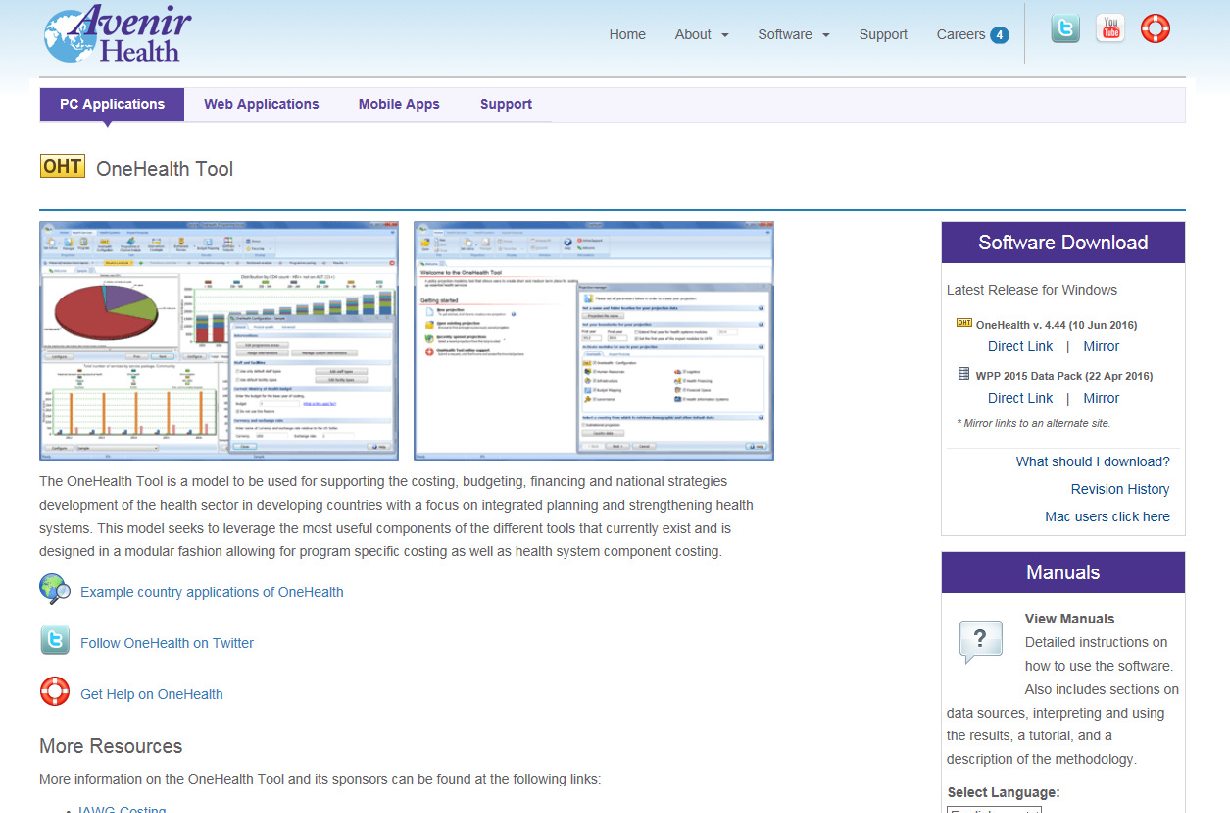
OneHealth Tool and Generalized Cost-Effectiveness Analysis
The OneHealth Tool (OHT) is a software package that is designed for strategic health planning in low- and middle-income countries. The OneHealth Tool incorporates demographic, disease and health system modules into one platform to produce evidence for interventions. Costs, budget impact, and systems requirements can be outputted; and when there are disease impact modules, cost-effectiveness analysis is feasible as well. As a result, the OHT is a tool that facilitates quantitative analysis of some of the most commonly used criteria in health priority-setting and benefit package design.
The OneHealth Tool is being rebuilt within an online platform and as part of this process, new information on health services and cost components will be imported from the UHC Compendium database.
Country contextualization of WHO-CHOICE cost-effectiveness analyses can also be conducted within the same platform using the Generalized Cost-Effectiveness Analysis (GCEA) tool. The tool is pre-populated with default country-specific data on prices, quantities and epidemiology, which are modifiable by the user. Contact the WHO CHOICE team at whochoice@who.int for more information.
Technical Capacity
Table: Courses and Training for Developing Capacity for HBP Design Processes
| Resource | Description | Reference |
1. IDB CRITERIA MOOC – What to Finance in Health and at What Price? | This online course features 7 modules that introduces the concepts around health benefit packages, explicit priority-setting processes, and instruments to achieve more affordable prices of medicines. The modules feature video lectures from experts in the field as well as exercises and exams to test one’s knowledge.
|
Available on EdX website: https://www.edx.org/course/what-to-finance-in-health-and-at-what-price and through the IADB CRITERIA website https://criteria.iadb.org/en. Note there is a free version and a paid version (with associated certificate) as of December 2021.
|
2. Case Studies in Making Fair Choices on the Path to Universal Health Coverage | This series of case studies follows from the WHO Making Fair Choices report and presents applied examples of specific problems and how they can be addressed with the fair choices framework. Each of the documents contains 3 case studies and discusses them according to: health benefit maximization, priority for the worse-off, financial risk protection, and finally providing a recommendation.
|
a. Voorhoeve, A., Tan-Torres Edejer, T., Kapiriri, L., Norheim, O.F., Snowden, J., Basenya, O., Bayarsaikhan, D., Chentaf, I., Eyal, N., Folsom, A. and Halina Tun Hussein, R., 2017. Making fair choices on the path to universal health coverage: applying principles to difficult cases. Health Systems & Reform, 3(4), pp.301-312. b. Voorhoeve, A., Edejer, T.T., Kapiriri, L., Norheim, O.F., Snowden, J., Basenya, O., Bayarsaikhan, D., Chentaf, I., Eyal, N., Folsom, A. and Hussein, R.H.T., 2016. Three case studies in making fair choices on the path to universal health coverage. Health and human rights, 18(2), p.11.
|
3. The Use of HTA to Achieve Universal Health Coverage | This is an onsite Summer course put on by Radboud University Medical Center. The course is designed for policy makers from ministries of health or other government institutions, HTA representatives, researchers and students, as well as industry representatives. There is a tuition fee for this course and registration is in May of each year. | Link to the course through the Radboud University website is here.
|
4. NIPH Report on Topic Identification, Selection and Prioritization (TISP) - 2021 | This paper presents cost-effectiveness estimates for non-communicable disease and mental health prevention, promotion and management interventions. | https://www.fhi.no/globalassets/bilder/rapporter-og-trykksaker/2021/topic-identification-selection-and-prioritisation-for-health-technology-assessment.pdf
|
Key WHO resources and/or selected non-WHO resources on inputs needed to support HBP design
Tools
|
| Resource | Description | Reference |
1. HIP Tool |
The HIPtool is an open access tool that allows for analyzing optimal resource allocation decisions. |
|
2. Bergen Center for Ethics and Priority Setting (BCEPS) FairChoices DCP Analytics Tool |
This tool, developed by researchers at the University of Bergen, provides a user-friendly way to visualize evidence on cost-effectiveness, equity impact and financial risk protection. | https://www.uib.no/en/bceps/130756/fairchoices-dcp-analytics-tool
|
Data Sources |
| Resource | Description | Reference |
3. The Tufts Medical Center CEA Registry | This is a comprehensive database of more than 10,000 cost-effectiveness analyses encompassing a broad range of diseases and treatments that have been published from 1976 until now. | https://cevr.tuftsmedicalcenter.org/databases/cea-registry
|
4. International HTA Database (hosted by INAHTA) | This is a freely accessible database of references to ongoing and published health technology assessments commissioned or conducted by HTA organisations worldwide. | https://database.inahta.org/
|
5. Disease Control Priorities (DCP) | DCP3 provides a comprehensive review of priority health interventions, including their efficacy, effectiveness, and cost-effectiveness. Additionally, DCP3 volumes provide systematic and standardized economic evaluations of specific interventions, delivery platforms, and policies. | http://dcp-3.org/ |


.jpeg?sfvrsn=22daf9da_1)
.png?sfvrsn=573ef12b_1)